When Sinus Surgery Fails: Missing Causes and Next Steps for Chronic Sinusitis
If you’re reading this, you may be frustrated, worried, or simply confused: you went through sinus surgery (such as Functional Endoscopic Sinus Surgery, FESS, or a balloon procedure), yet you still have congestion, drainage, pressure, or repeat “sinus infections.” It’s common to describe this experience as failed sinus surgery—but in real life, “failure” usually has a reason.
This guide is educational and patient-focused. It’s meant to help you understand why symptoms can persist and what kinds of next steps are typically considered in a thoughtful, step-by-step workup.
A quick reassurance—sinus surgery “failure” isn’t always a dead end
What “failed sinus surgery” usually means (and what it doesn’t)
Most of the time, failed sinus surgery means one of these:
- Symptoms never improved after surgery
- Symptoms improved for a while, then gradually returned
- Infections became less frequent, but daily quality-of-life symptoms linger (congestion, mucus, smell loss, facial fullness)
Importantly, this does not automatically mean the surgery was “botched.” Chronic rhinosinusitis (CRS) is often multi-factorial—meaning anatomy, inflammation, allergies, immune factors, and healing patterns can all contribute.
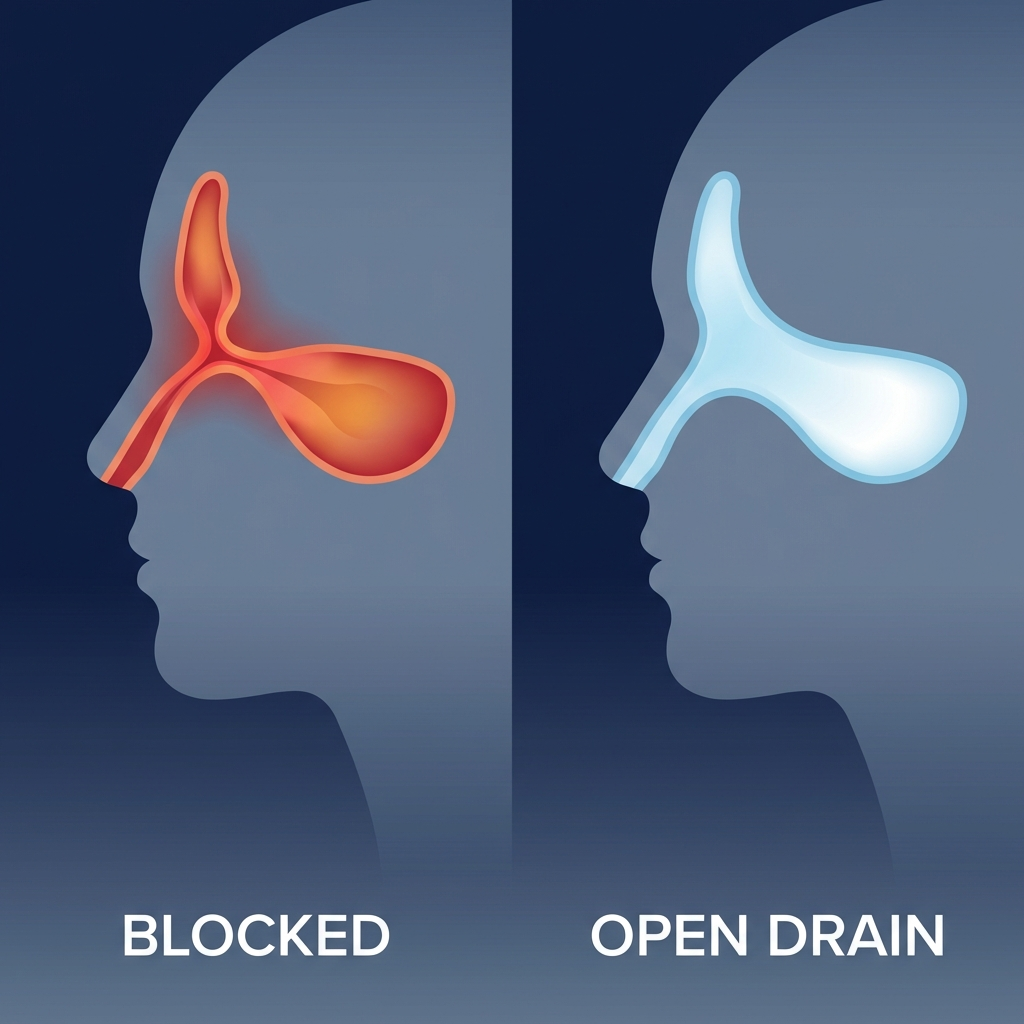
A useful analogy: surgery can widen the drainage pathways, but if the lining keeps swelling (inflammation) or if healing narrows the opening again (scar), the “drain” may still not work the way you expected.
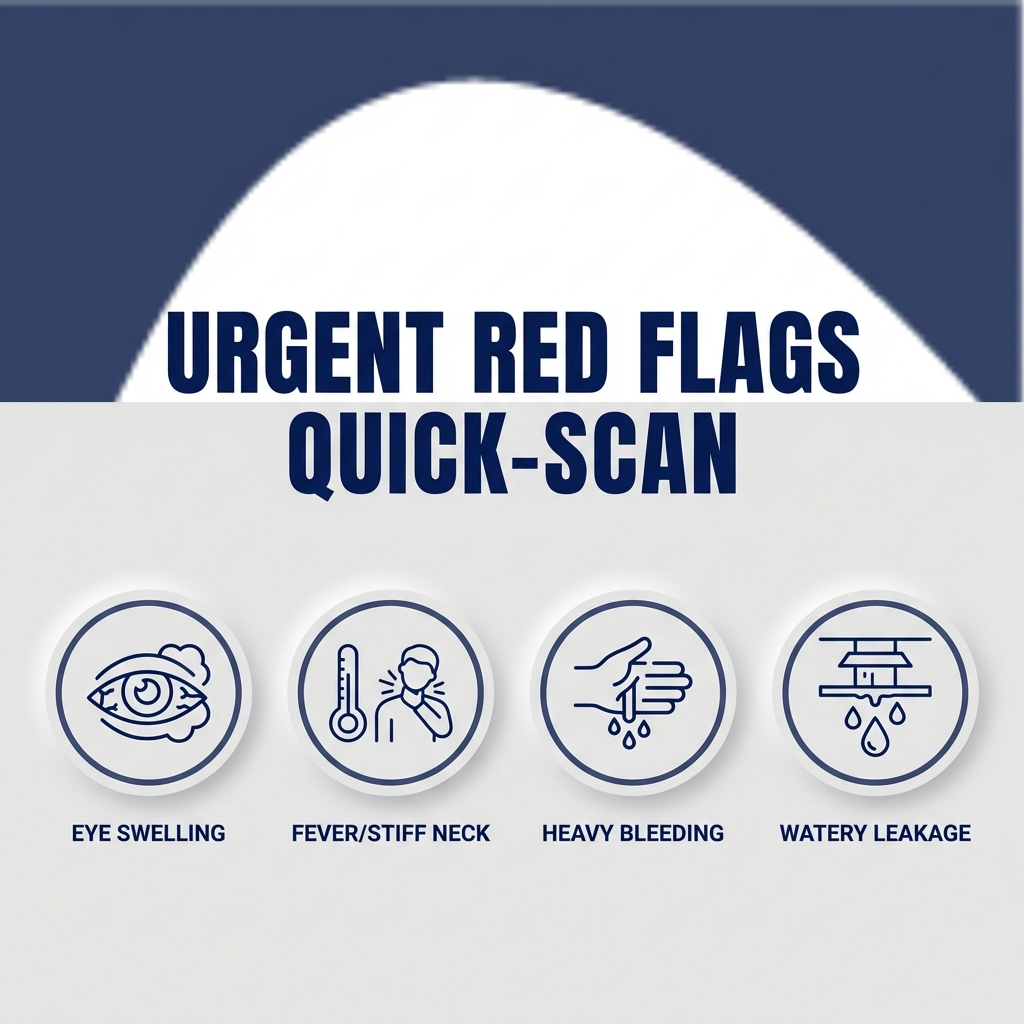
When to worry right away (urgent red flags)
Urgent evaluation is commonly recommended for symptoms that could signal a complication or a non-sinus emergency, such as:
- Swelling around the eye, eye pain, bulging, or vision changes
- Severe headache with fever, stiff neck, confusion, or marked lethargy
- Heavy nosebleeds that won’t stop
- Clear, watery drainage that seems unusual (especially after trauma)
If you or someone else has any of these urgent symptoms, seek emergency medical care immediately.
Symptoms checklist—are you dealing with true sinus inflammation or something else?
Common ongoing symptoms after sinus surgery
Whether the issue is inflammation, anatomy, or something else, people with persistent symptoms after sinus surgery often report:
- Nasal blockage/congestion
- Postnasal drip or thick mucus
- Reduced smell/taste
- Facial pressure/fullness
- Recurrent “sinus infections” and multiple antibiotic courses
- Cough, throat clearing, fatigue, bad breath
A common phrase is: “I can breathe for a few days, then it all closes back up.” That pattern can happen with recurring inflammation, not just mechanical blockage.
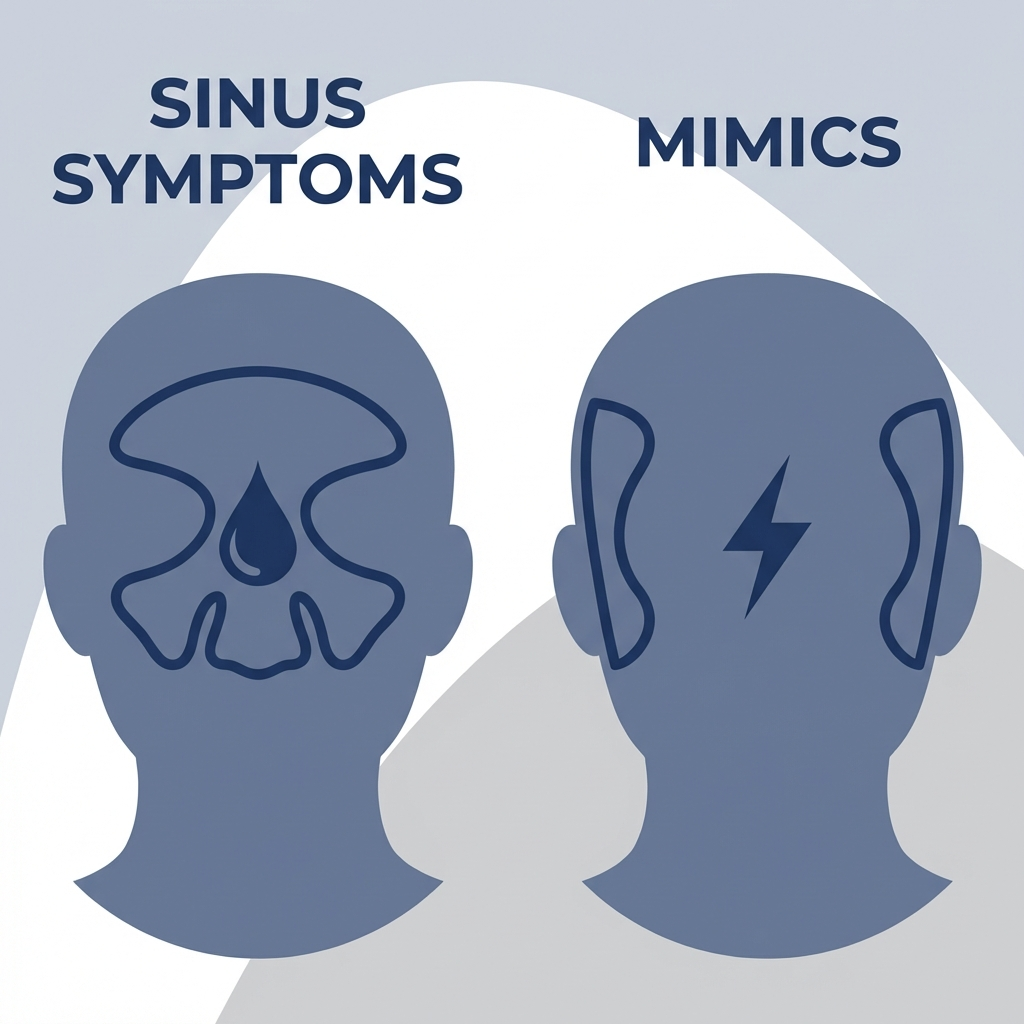
Clues your symptoms may not be primarily sinusitis
Some symptom patterns point away from the sinuses as the main cause:
- Facial “pressure” without much congestion or mucus (migraine or TMJ-related pain can mimic sinus pressure)
- Clear runny nose triggered by temperature changes, exercise, or spicy foods (often nonallergic/vasomotor rhinitis)
- Burning/irritation with a normal or near-normal CT scan (irritants, dryness, rhinitis)
Clinical note (patient-friendly): many people label facial pain as “sinus pressure,” but facial pain can come from non-sinus causes—even after a technically successful sinus procedure.
For a broader overview of CRS symptoms and diagnosis, see our guide: https://sleepandsinuscenters.com/chronic-sinusitis
*If your symptoms don’t match typical CRS patterns, redirecting the workup often leads to faster answers and better results.*

Why sinus surgery can fail—big picture causes (the 5-bucket framework)
When sinus surgery didn’t deliver lasting relief, clinicians often sort the causes into five practical “buckets.” This approach helps turn a frustrating situation into an organized plan—so you’re not just cycling through another round of antibiotics “just in case.”
Quick map: common patterns and what gets checked next
- One-sided blockage or a “mechanically blocked” sensation → Anatomy/scar → Nasal endoscopy ± CT
- Forehead pressure or recurrent frontal infections → Frontal narrowing/stenosis → Endoscopy + CT focused on the frontal recess
- Smell loss with recurring polyps → Inflammation/polyps → Endoscopy + CT; planning long-term anti-inflammatory care
- Thick drainage that keeps returning → Biofilm/resistant infection → Endoscopy; sometimes culture-directed therapy
- Persistent symptoms but imaging looks mild → Not only sinusitis (rhinitis/migraine/TMJ/reflux) → Targeted evaluation based on symptoms
Bucket 1 — Technical/anatomical problems (things that block drainage again)
Even after a well-performed procedure, airflow and drainage pathways can narrow again or remain partially obstructed, for example:
- Residual air cells or incomplete opening (such as persistent ethmoid partitions)
- Scar tissue/adhesions (synechiae) that tether tissue and block flow
- Narrowed sinus openings (stenosis), especially in the frontal sinus area
- Persistent septal deviation or turbinate issues contributing to obstruction
Bucket 2 — Disease persistence/recurrence (the underlying condition keeps going)
Some forms of CRS are driven by ongoing inflammation that surgery can’t “cure” by itself. Examples include:
- Nasal polyp regrowth (common in CRS with nasal polyps)
- Biofilms, where bacteria live in protective communities that are harder to eradicate
- Resistant organisms or, in select cases, fungal disease patterns
Bucket 3 — Patient-specific drivers that weren’t fully treated
A very common reason for chronic sinusitis after surgery is that the “driver” of inflammation wasn’t fully identified or controlled:
- Undertreated allergies
- Immune deficiencies (leading to frequent infections)
- Asthma or aspirin-exacerbated respiratory disease (AERD)
- Incomplete post-op care or challenges with medication routines (rinses, topical steroids, follow-up)
Bucket 4 — Limitations of the first surgery or mismatched procedure choice
Sometimes the first procedure was intentionally conservative, or it didn’t address the most involved areas:
- Only one or two sinuses were treated, while others remained blocked
- Frontal sinus access may have been limited (frontal pathways are delicate and complex)
- Balloon-only approaches can help select anatomy, but may not address more extensive tissue disease in others
For a patient-friendly ESS overview, see: https://sleepandsinuscenters.com/blog/endoscopic-sinus-surgery-what-patients-should-know
Bucket 5 — Not sinusitis (or not only sinusitis)
Finally, some ongoing symptoms are real—but not primarily caused by sinus inflammation:
- Allergic or nonallergic chronic rhinitis (a very common mimic)
Learn more: https://sleepandsinuscenters.com/treating-chronic-rhinitis
- Migraine or atypical facial pain
- TMJ dysfunction
- Reflux-related throat symptoms that feel like postnasal drip
- Environmental irritants (smoke, fragrance, workplace exposure)
*Putting symptoms into the right bucket prevents trial-and-error care and helps you target the true cause faster.*
The most commonly “missed” anatomical issues after surgery (and how they’re found)
Scar tissue/adhesions (synechiae)
After surgery, nearby surfaces can occasionally heal together, forming a band of scar tissue. This can:
- Reduce nasal airflow
- Block medication delivery (sprays/rinses don’t reach the target)
- Create a “closed-off” feeling—sometimes more on one side than the other
These are typically identified with nasal endoscopy in the office.
Narrowed sinus openings (stenosis)—especially frontal sinus
The frontal sinus drainage pathway is narrow and can re-narrow during healing. When it does, symptoms may include:
- Forehead pressure/fullness
- Repeat frontal infections
- Symptoms that fluctuate with inflammation flare-ups
Endoscopy plus an updated CT can show whether the frontal drainage route is open.
Residual ethmoid cells/incomplete ethmoidectomy
Ethmoid sinuses are made of many small partitions. If inflamed partitions remain, they can continue to swell and produce mucus, contributing to ongoing symptoms.
Septum/turbinate contributors that still matter post-surgery
Sinus surgery can open the sinuses, but if nasal airflow is still limited by a deviated septum, turbinate hypertrophy, or nasal valve narrowing, you may still feel “stuffy” even when the sinuses themselves are better. Endoscopy and a careful nasal exam help sort this out.
*When anatomy is the issue, seeing it clearly on endoscopy or CT makes the next step much more straightforward.*
Disease that comes back: polyps, biofilms, and “stubborn inflammation”
Nasal polyps—why they regrow and what that means for long-term care
For many patients, surgery is best viewed as creating space and access—space for breathing and drainage, and access so topical medications can reach deeper areas. But it doesn’t remove the body’s tendency toward inflammation. That’s why the underlying inflammatory condition often needs a long-term maintenance plan.
Biofilms and resistant bacteria—why antibiotics may stop helping
Biofilms are communities of bacteria that form a protective layer. They can be harder for antibiotics (and even immune defenses) to fully eliminate. When symptoms keep returning after multiple antibiotics, clinicians often shift toward endoscopy-guided evaluation and, in selected cases, culture-directed therapy. In some situations, antibiotics still help—especially when targeted by culture results and combined with topical anti-inflammatory care.
When to consider newer therapies (biologics, steroid irrigations)
For certain severe polyp-driven cases, modern options may be discussed, such as:
- High-volume steroid irrigations (topical anti-inflammatory therapy delivered deeper than a spray)
- Biologic medications for selected patients with severe nasal polyps and related inflammatory disease (specialist-prescribed and monitored)
*If inflammation is the driver, the best results usually come from pairing good sinus access with the right long-term anti-inflammatory plan.*
Patient factors that can sabotage results (even with a technically good surgery)
Allergies that weren’t diagnosed—or weren’t controlled
Allergies can keep the nasal lining swollen and reactive, increasing congestion and mucus even when the sinuses are surgically open. If you’ve never been tested, this can be a high-value next step: https://sleepandsinuscenters.com/allergy-testing
Immune deficiency—when recurrent infections suggest an immune workup
Some people with frequent infections have an immune issue such as low immunoglobulins or an impaired antibody response to vaccines. In these situations, patients may hear about tests like:
- Quantitative immunoglobulins (IgG, IgA, IgM)
- Vaccine antibody responses (how well the immune system responds)
Asthma/AERD and other inflammatory conditions
In patients with asthma, nasal polyps, or AERD, the nose and lungs can be part of a connected inflammatory system. Coordinated care can matter because controlling overall inflammation often improves both nasal and breathing symptoms.
Follow-through and healing (the “aftercare” part of sinus surgery success)
Post-operative care is part of the procedure’s success—especially early on. Saline rinses, topical medications, and follow-up visits can help reduce crusting and inflammation while healing occurs. When aftercare is difficult to complete, scarring and narrowing risks can increase.
*Finding and treating the “driver” behind your inflammation may be the single most important step after surgery.*

What to do next—step-by-step evaluation after failed sinus surgery
A structured re-evaluation usually helps more than guessing.
Step 1 — Clarify the timeline and pattern of symptoms
Patterns offer clues:
- Better immediately after surgery, then worse: sometimes scarring/stenosis or recurrence
- Never improved: consider an incomplete target, a missed driver (like allergies), or a non-sinus cause
Step 2 — Nasal endoscopy in the office
Endoscopy can show:
- Polyps
- Drainage or pus
- Scar bands/adhesions
- Swollen tissue blocking key pathways
Step 3 — Updated sinus CT scan (when indicated)
CT can help identify:
- Blocked sinus openings
- Retained partitions/cells
- Persistent inflammation patterns
- Frontal sinus pathway problems
Step 4 — Targeted testing based on suspicion
Depending on what’s found, next steps may include allergy testing, cultures, or broader evaluation when imaging is mild. Explore CRS basics: https://sleepandsinuscenters.com/chronic-sinusitis
*Objective findings on endoscopy/CT plus targeted testing will keep your plan precise and personalized.*

Treatment options when sinus surgery fails (starting with least invasive)
A key takeaway: many cases of persistent symptoms after sinus surgery improve by tightening the diagnosis and optimizing medical therapy—especially therapies that reduce inflammation and improve nasal hygiene.
Optimize medical therapy (often the biggest missing piece)
Common categories discussed in post-surgery care include:
- Daily saline irrigations (often high-volume)
- Intranasal steroid sprays and/or steroid irrigations
- Short oral steroid courses in selected situations (only under medical supervision due to potential risks)
- Antibiotics only when bacterial infection is likely (often culture-guided when drainage persists)
- Treatments for rhinitis (allergic/nonallergic), depending on the trigger pattern
Learn more about chronic rhinitis options: https://sleepandsinuscenters.com/treating-chronic-rhinitis
Address the driver—targeted add-ons
Examples of “driver-focused” approaches:
- Allergy management (avoidance, medications, and in some cases immunotherapy)
- Coordinated management when asthma/AERD is present
- Culture-directed strategies when drainage persists or returns frequently
In-office procedures that may help select patients
In some cases, clinicians may discuss:
- Debridement to remove crusting and help healing
- Balloon dilation for focal narrowing in select anatomy patterns
- Steroid-eluting implants in selected cases
When revision sinus surgery makes sense (and when it doesn’t)
Revision sinus surgery is usually considered when there is objective evidence of a correctable problem—seen on endoscopy and/or CT—such as:
- Scar-related blockage
- Narrowed openings that won’t stay open
- Persistent diseased partitions/cells
- Recurrent polyps causing obstruction
The goal is to restore ventilation/drainage and improve medication delivery—not to promise a guaranteed cure.
*The right mix of hygiene, anti-inflammatory therapy, and targeted procedures typically outperforms repeating antibiotics alone.*
Lifestyle and home tips to support healing and reduce flare-ups
Daily habits that reduce inflammation burden
- Consistent saline rinsing routine
- Correct nasal spray technique (often taught as aiming slightly outward, away from the septum)
- Hydration and humidification in dry environments
Reduce environmental triggers
- Avoid smoke/vaping exposure
- Minimize fragrance exposure if sensitive
- Track air quality and consider basic filtration strategies at home
If symptoms are “pressure headaches,” try symptom-tracking tips
A simple diary can help separate sinus flares from headache patterns:
- Weather shifts, sleep changes, stress
- Specific foods or dehydration
- Response (or lack of response) to typical sinus medications
This can guide whether migraine/TMJ evaluation should be part of the plan.
*Small daily changes often reduce swelling and improve how well your medications—and your surgery—can work.*
FAQs about persistent symptoms after sinus surgery
How long does it take to feel normal after sinus surgery?
Healing varies. Many people feel gradual improvement over weeks, but inflammation can take longer to settle—especially in polyp disease or allergy-driven swelling. Follow-up matters because healing changes can be addressed early. For a patient-friendly ESS overview, read: https://sleepandsinuscenters.com/blog/endoscopic-sinus-surgery-what-patients-should-know
Is it normal to still have congestion months later?
It can be, particularly with allergies, rhinitis, or recurring polyps. Ongoing congestion months later is often a reason to reassess the diagnosis and confirm whether there’s inflammation, scarring, or a non-sinus contributor.
Do nasal polyps always come back?
Not always, but recurrence risk is real in certain inflammatory types of CRS. Long-term maintenance therapy is often part of preventing regrowth.
Could my problem be allergies if I had surgery?
Yes. Surgery can improve airflow and medication access, but it doesn’t remove allergic tendency. If allergies haven’t been evaluated, consider: https://sleepandsinuscenters.com/allergy-testing
When do you consider revision surgery?
Often when symptoms persist and there is objective evidence of obstruction or persistent disease on endoscopy/CT despite optimized medical therapy.
What should I bring to my second-opinion visit?
Helpful items include:
- Prior operative report (if available)
- Prior CT images/reports (actual images are ideal)
- A current medication list
- Allergy history/testing results
- A timeline of antibiotics and steroid courses
Call to action—get a targeted second look (not another guess)
If you believe you’ve had failed sinus surgery—or you’re dealing with chronic sinusitis after surgery—the most productive next step is usually a targeted re-evaluation: careful symptom review, nasal endoscopy, and an evidence-based plan that matches the cause (anatomy, inflammation, allergy, immune factors, or a non-sinus diagnosis).
To schedule a visit, you can book an appointment here: https://www.sleepandsinuscenters.com/
Helpful next reading
- What endoscopic sinus surgery involves and recovery expectations: https://sleepandsinuscenters.com/blog/endoscopic-sinus-surgery-what-patients-should-know
- CRS overview: https://sleepandsinuscenters.com/chronic-sinusitis
- Chronic rhinitis options: https://sleepandsinuscenters.com/treating-chronic-rhinitis
- Allergy testing: https://sleepandsinuscenters.com/allergy-testing
*A careful second look can reveal the true reason for persistent symptoms—and a clearer path forward.*
Citations
1. Ramadan HH. Reasons for failure in endoscopic sinus surgery. https://pubmed.ncbi.nlm.nih.gov/9917035/
2. Richtsmeier WJ. (Persistent symptoms/failure factors literature). https://pubmed.ncbi.nlm.nih.gov/11801976/
3. Refractory chronic rhinosinusitis and revision considerations. https://link.springer.com/article/10.1007/s40136-012-0004-3
4. Operative Techniques in Otolaryngology—revision/failure discussion. https://www.optecoto.com/article/S1043-1810(06)80009-6/fulltext
5. University of Iowa repository summary on failure reasons. https://iro.uiowa.edu/esploro/outputs/journalArticle/Reasons-for-Failure-in-Endoscopic-Sinus/9984303904502771
Disclaimer: This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.