Red Flags in Chronic Sinus Disease: Warning Signs You Shouldn’t Ignore
Chronic sinus symptoms are incredibly common—and they can be frustrating, exhausting, and disruptive. Most of the time, they’re related to ongoing inflammation in the nose and sinuses (not an emergency). But in some situations, chronic sinus complaints can overlap with, or mask, more serious problems.
This guide is designed to help you understand what’s typical, what may be a red flag in chronic sinus disease, and how to think about the “where should I go?” question (ER vs. urgent care vs. ENT). It’s educational information—not a diagnosis or personalized medical advice.
A simple way to frame it: chronic sinus symptoms can be “background noise” you learn to live with—until something changes. Red flags are those “something changed” moments.
What Counts as “Chronic” Sinus Disease?
Chronic sinusitis definition (the 12-week rule)
In general, sinus symptoms lasting 12 weeks or longer are considered “chronic,” meaning there is ongoing inflammation rather than a short-lived infection. This “12-week rule” is commonly used in public health and clinical guidance. [1][2]
Think of it like a sprained ankle: a few days of swelling is expected, but swelling that lingers for months signals an ongoing issue that may need a different approach.
If you want a deeper overview of symptom patterns, you can compare your experience with this list of symptoms of sinus problems: https://sleepandsinuscenters.com/symptoms-of-sinus-problems

Common (non-emergency) chronic sinus symptoms
Chronic sinus disease often includes symptoms like:
- Nasal congestion or blockage
- Thick drainage (from the nose or down the throat)
- Facial pressure or fullness
- Reduced smell and taste
- Cough, bad breath, fatigue
These symptoms can feel intense and still be non-emergent. For example, it’s common to feel “clogged,” sleep poorly, and wake up with throat-clearing from post-nasal drip—without having a dangerous infection.
The key question is whether anything suggests a complication, a different diagnosis, or a sudden escalation from your usual baseline.
- In short: chronic symptoms that are stable and familiar usually allow for planned care; a sudden change or new, severe symptom deserves faster attention.
Red Flags vs. Typical Symptoms (Quick Guide)
“Yellow light” vs. “Red light” symptoms
A helpful way to think about red flags in chronic sinus disease is to separate “persistent but expected” symptoms from symptoms that could signal a more urgent situation.
- Yellow light (watch closely / plan next steps): persistent congestion, pressure, reduced smell, ongoing post-nasal drip
- Red light (urgent evaluation): neurologic changes, eye symptoms, high fever, severe or rapidly worsening swelling or pain, stiff neck, or a “got better and then worse again” pattern
One clinician-style rule of thumb: if your symptoms are “the same old story,” you can usually plan care. If you’re thinking, “This is different,” it’s time to reassess.
Quick triage checklist (easy scanning)
- Vision changes or double vision: possible involvement near the eye socket. Action: urgent or emergency evaluation may be needed.
- Eye swelling/redness (especially one-sided) or pain with eye movement: possible orbital inflammation/infection. Action: urgent or emergency evaluation may be needed.
- Confusion, extreme drowsiness, difficulty speaking/walking: possible neurologic complication. Action: emergency evaluation may be needed.
- Stiff neck (especially with fever/headache): possible serious infection involvement. Action: emergency evaluation may be needed.
- Fever over 102°F / 39°C: more concerning systemic illness. Action: same-day evaluation (urgent care/doctor). Note: lower-grade fever paired with worsening symptoms or risk factors may still warrant prompt care.
- New, sharp, or rapidly worsening facial pain/swelling (especially if different from your usual pattern): could indicate a complication or severe inflammation. Action: same-day evaluation.
- Symptoms that improve temporarily and then worsen again (“double worsening”): can signal a bacterial shift or complication. Action: prompt reassessment.
- Recurrent infections or not improving with treatment: suggests ongoing inflammation or structural blockage. Action: consider ENT referral for sinusitis.
- Bottom line: if symptoms are new, sharply worse than usual, or include eye/neurologic changes, treat them as urgent until proven otherwise.
Emergency Red Flags (Go to the ER / Call Emergency Services)

Some chronic sinusitis warning signs are treated as emergencies because, in rare cases, infection or inflammation can extend beyond the sinuses. When that happens, it may affect areas around the eyes or the tissues surrounding the brain. [3][4]
For an expanded explanation of how this happens, see: https://sleepandsinuscenters.com/blog/can-a-sinus-infection-spread-signs-to-watch/
Neurological symptoms (don’t wait)
Symptoms that deserve urgent attention include:
- New confusion or disorientation
- Difficulty speaking, walking, new weakness, or unusual coordination issues
- Extreme drowsiness or being difficult to wake
- A severe, persistent headache that feels different from your usual pattern
Why this matters: these can be associated with serious complications such as meningitis or a brain abscess (both uncommon, but time-sensitive). [3][4]
Concrete example: if you usually get “sinus pressure headaches” across your cheeks, but this time you have a severe headache plus confusion or you can’t stay awake—treat that as an emergency-level change.
Vision or eye-area changes
This category is especially important because the sinuses sit close to the eye socket. Concerning symptoms include:
- Double vision, blurry vision, or reduced vision
- Eye pain (especially with movement)
- Swelling/redness around the eye or eyelids, especially if worsening or one-sided
Why this matters: this may indicate orbital complications (infection/inflammation near the eye). [3][4]
A practical comparison: mild under-eye puffiness from poor sleep is common. New, painful, one-sided eyelid swelling—especially with fever or vision changes—is not.
Stiff neck (especially with fever/headache)
A stiff neck—particularly when paired with fever, headache, or light sensitivity—can be a warning sign that needs emergency-level evaluation. [3][4]
If you’re unsure when to go to the ER for sinus symptoms, eye changes plus neurologic symptoms plus stiff neck are the clearest “do not wait” group.
- If eye symptoms or neurologic changes show up suddenly or alongside fever and a stiff neck, seek emergency care immediately.
Urgent Red Flags (Same-Day Care: Urgent Care or Prompt Doctor Visit)

Not every concerning symptom requires an ER, but some deserve same-day evaluation—especially if they’re escalating quickly.
High fever or severe systemic illness
Fever is not always prominent in chronic sinusitis. A high fever (over 102°F / 39°C), chills, or appearing very ill is a reason to consider prompt medical assessment. [2][3] Lower-grade fever combined with rapidly worsening symptoms or higher-risk health conditions may also warrant same-day care.
Severe or worsening facial pain/swelling
Facial pain and pressure can be part of chronic disease—but new, sharp, or rapidly worsening pain or visible swelling (especially if localized to one cheek or different from your typical pattern) should be reassessed quickly. [2][3]
“Double worsening” pattern (improve, then worsen again)
If symptoms improve and then suddenly worsen again—sometimes described as “double worsening”—this can signal a change in what’s driving symptoms and is worth timely follow-up. [1][3]
- Treat same-day red flags as a signal to get care now rather than “wait and see.”
Red Flags Over Time (When It’s Not an Emergency—but Still Needs ENT Evaluation)
Symptoms that don’t respond to standard treatment
If you’ve tried clinician-recommended therapies (for example: consistent saline rinses, nasal steroid sprays, or other appropriate steps) and there’s little improvement, that’s often the moment to consider an ENT referral for sinusitis.
Learn more about evaluation and treatment options for chronic sinusitis here: https://sleepandsinuscenters.com/chronic-sinusitis
Frequent recurrences
Several infections per year—or a cycle of constant flare-ups—can suggest an underlying driver such as uncontrolled inflammation, polyps, allergies, or an anatomic drainage issue.
In plain terms: if you feel like you’re always “almost better but never well,” it’s reasonable to ask what’s keeping the cycle going.
One-sided or unusual symptoms
Symptoms that are consistently one-sided or unusual should be assessed, especially if they persist. Examples include:
- Ongoing one-sided blockage or drainage
- Recurrent nosebleeds on one side
- New facial numbness or unusual pressure pattern
These are not automatically dangerous, but persistent or unusual unilateral symptoms always require professional assessment to rule out less common causes.
- If symptoms keep recurring, resist the urge to normalize them—ask why they’re happening and whether something is being missed.
Why These Red Flags Matter (Potential Complications Explained Simply)
How a sinus infection can spread
Sinuses are air-filled spaces in the bones of the face. Because they’re close to the eyes and the brain, severe infection (rarely) can extend beyond the sinus cavity. [3][4] That’s the main reason red flags in chronic sinus disease matter.
An easy analogy: the sinuses are like rooms in a house. Most of the time, the issue stays “in the room.” Rarely, it can affect the “next door” areas—like the eye socket or nearby tissues—which is why certain symptoms raise urgency.
Examples of serious complications (plain language)
While uncommon, complications can include:
- Orbital cellulitis/abscess: infection near or within the eye socket
- Meningitis: infection/inflammation of the lining around the brain/spinal cord
- Brain abscess: a pocket of infection in brain tissue
These are not the typical outcome of sinus problems—but recognizing warning signs helps people seek timely evaluation. [3][4]
- Serious complications are rare, but acting quickly on red flags is what keeps rare events from becoming dangerous.
Common Causes & Risk Factors That Can Make Chronic Sinus Disease Harder to Treat
Inflammation drivers (common)
- Allergies or chronic rhinitis
- Nasal polyps
- Asthma and related inflammatory conditions (in some people)
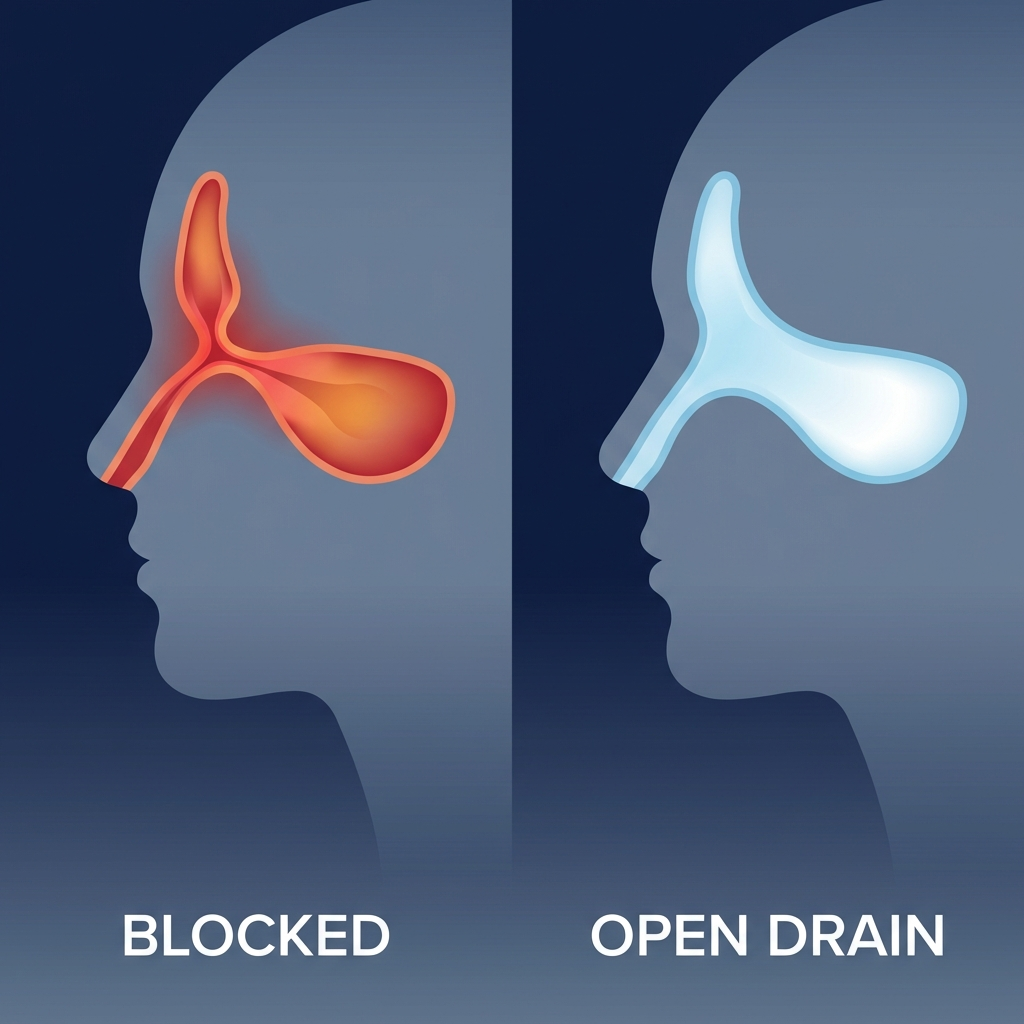
Structural contributors
- Deviated septum
- Narrow drainage pathways
- Changes from prior trauma or surgery
Health factors that raise concern for complications
Some health situations can raise concern for more severe infection or slower healing, such as:
- Weakened immune system
- Uncontrolled diabetes
- Smoking/vaping exposure
- Significant untreated dental infections (upper teeth)
If any of these apply to you, it doesn’t mean something dangerous is happening—it simply lowers the threshold for getting checked sooner when symptoms change.
- Knowing your risk factors helps you decide sooner when a change deserves attention.
What to Do If You Notice a Red Flag (Step-by-Step)
Decide where to go (practical triage)

This is a general way to think about triage (not a substitute for professional judgment):
- ER now: confusion, vision changes/double vision, stiff neck, severe eye swelling/redness [3][4]
- Same-day urgent care/doctor: fever over 102°F, new or rapidly worsening facial pain or swelling, symptoms that improved and then worsened again [2][3]
- Schedule ENT: symptoms lasting 12+ weeks, frequent recurrences, or symptoms that are treatment-resistant [1][2]
What to tell the clinician (to speed up care)
When you’re being evaluated, it can help to share:
- Your symptom timeline (start date and whether you improved then worsened)
- Your highest recorded temperature
- Any eye or neurologic symptoms (even if they come and go)
- What you’ve already tried (rinses, sprays, antibiotics, steroids, allergy meds)
A brief “script” can help: “This has been going on since October, I improved last week then worsened two days ago, my highest fever was 102.4, and today my right eyelid is swollen.”
What not to do
- Avoid using leftover antibiotics or someone else’s prescription; they don’t treat viral infections, can mask important symptoms, and increase side effects and antibiotic resistance.
- Be cautious with topical decongestant sprays; frequent use can cause rebound congestion.
- If you’re unsure where to go, err on the side of urgent care or the ER for eye or neurologic changes, and schedule ENT for persistent or recurring problems.
How Chronic Sinus Disease Is Evaluated by an ENT

Office evaluation
An ENT visit typically includes:
- A detailed symptom and health history
- An exam of the nose and throat
- Sometimes a nasal endoscopy (a small camera used to look deeper inside the nasal passages)
Many patients find it reassuring to hear some version of: “Let’s confirm what type of inflammation you have and whether anything is blocking drainage,” rather than guessing based on symptoms alone.
Imaging and tests (when indicated)
Depending on symptoms and history, an ENT may recommend:
- A CT scan to look for inflammation patterns or blockage
- A culture in persistent or resistant cases
- Allergy testing when triggers are suspected
- A focused ENT exam clarifies what’s driving symptoms so treatment can be matched to the cause.
Treatment Options (From Conservative to Advanced)
At-home and OTC basics (when appropriate)
Many care plans include foundational steps such as:
- Saline irrigation
- Hydration and humidification
- Avoiding irritants (smoke, strong fragrances) and known allergy triggers
Medical treatments your clinician may recommend
Depending on the situation, treatment can include:
- Intranasal corticosteroid sprays or rinses
- Antibiotics only when appropriate (not all sinus infections require them) [1]. Many sinus infections are viral or primarily inflammatory; antibiotics are reserved for confirmed or strongly suspected bacterial infections.
- Short courses of oral steroids in selected cases (provider-guided)
When procedures or surgery enter the conversation
If symptoms persist due to blockage or ongoing inflammation, procedures such as balloon sinuplasty or endoscopic sinus surgery may be discussed. The goal is to improve drainage/ventilation and reduce flare frequency—not simply to “treat a cold.”
For an overview of chronic sinusitis care and when procedures are considered, visit: https://sleepandsinuscenters.com/chronic-sinusitis
- Most people improve with targeted medical therapy; procedures are considered when anatomy or persistent inflammation keeps the cycle going.
Lifestyle Tips to Reduce Flares (and Catch Changes Early)
Build your “baseline” symptom tracker
A quick daily note—congestion level, smell, facial pain, sleep quality—can make it easier to notice changes that might represent red flags in chronic sinus disease rather than your usual baseline.
Reduce inflammation triggers
- Keep allergy routines consistent when allergies are part of the picture
- Improve indoor air quality (filters, humidity balance, mold awareness)
Sleep and hydration habits that support mucus health
- Adequate fluids
- Manage dry indoor air
- Avoid smoke exposure
- A simple daily log helps you spot “not my normal” patterns early, when action matters most.
FAQs (Patient-Focused)
When is sinusitis considered chronic?
When symptoms last 12 weeks or longer. [1][2]
When should I go to the ER for sinus symptoms?
In general, ER-level warning signs include vision changes, confusion/extreme drowsiness, stiff neck, or significant eye swelling/redness. [3][4]
Can chronic sinusitis cause headaches every day?
It can contribute to headaches, but daily headaches can also have other causes—evaluation helps clarify what’s driving symptoms.
Why do my symptoms keep coming back?
Common reasons include allergies, nasal polyps, anatomic blockage, or incomplete control of inflammation. [1][2]
Do I always need antibiotics?
No. Many sinus infections are viral or primarily inflammatory, so antibiotics are used only when bacterial infection is confirmed or strongly suspected. [1]
What if my symptoms improved then suddenly got worse?
That “improved, then worsened” pattern (“double worsening”) is worth prompt reassessment. [3]
- If a question keeps coming up for you, that’s a sign it’s worth discussing with an ENT so you can get a tailored plan.
Conclusion + Clear Call to Action
Chronic congestion and pressure are common—but red flags are not. Knowing the difference can help you choose the right level of care, especially when symptoms change quickly or include eye or neurologic concerns.
If you’ve had sinus symptoms for 12+ weeks, they keep coming back, or they’re not improving with standard steps, schedule an ENT evaluation. To get started, you can book an appointment with Sleep and Sinus Centers of Georgia here: https://www.sleepandsinuscenters.com/
Citations
1. CDC – Sinus Infection (Sinusitis): https://www.cdc.gov/sinus-infection/about/index.html
2. NHS – Sinusitis (sinus infection): https://www.nhs.uk/conditions/sinusitis-sinus-infection/
3. Mayo Clinic – Sinusitis symptoms / when to seek care: https://www.mayoclinic.org/diseases-conditions/acute-sinusitis/symptoms-causes/syc-20351671
4. Doctor On Demand – When to go to the ER for a sinus infection: https://doctorondemand.com/blog/cold-and-flu/when-to-go-to-the-er-for-a-sinus-infection/
5. ENT Doctors Los Angeles – When sinus symptoms mask something more serious: https://entdoctorslosangeles.com/when-sinus-symptoms-mask-something-more-serious-ent-signs-you-shouldnt-ignore/
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.