Can Autoimmune Diseases Cause Sinus Inflammation? Symptoms, Causes, and Treatment
Chronic nasal congestion and “sinus infections” that keep coming back are often blamed on allergies or germs. But for a smaller group of people, the driver is the immune system itself. Autoimmune sinus inflammation can look like typical sinus trouble at first—until it doesn’t respond the way you’d expect.
This article explains how autoimmune disease can affect the nose and sinuses, what symptoms can be more suggestive of an autoimmune cause, how evaluation typically works, and what treatment approaches are commonly used.
Medical disclaimer: This article is for general education and is not a substitute for personal medical advice, diagnosis, or treatment. If you have persistent, worsening, or unusual symptoms—especially bleeding, severe pain, or symptoms outside the nose/sinuses—seek timely care from a qualified clinician.
Note: “Autoimmune sinus inflammation” is a descriptive term used here to explain when autoimmune diseases affect the sinuses. It is not a formal diagnosis, but a clinical pattern that warrants further evaluation.
Quick Answer: Yes—Autoimmune Disease Can Cause Chronic Sinus Inflammation
Autoimmune diseases occur when the immune system mistakenly attacks healthy tissue. When that “misfire” involves the lining of the nose/sinuses (and sometimes the small blood vessels or cartilage in that area), it can lead to ongoing inflammation rather than a short, self-limited illness.
A helpful analogy: if your immune system is like a smoke alarm, autoimmune disease can act like a sensor that’s set too “sensitive.” Instead of sounding only during a real fire (an infection), it may keep going even when there’s no smoke—creating persistent swelling and irritation.
The challenge is that autoimmune-related sinus problems can mimic allergies or infections, yet may not improve with typical treatments like antihistamines or repeated antibiotics—because the main issue isn’t a new germ or seasonal pollen exposure. Researchers have also described meaningful overlap between chronic rhinosinusitis inflammatory pathways and the immune dysregulation seen in autoimmune diseases. [1]
Autoimmune or immune-mediated conditions that are commonly associated with nasal/sinus inflammation include:
- Granulomatosis with Polyangiitis (GPA) (a type of vasculitis that can affect the upper airways) [3]
- Sarcoidosis (granulomas that can involve the nasal passages/sinuses) [2]
- Systemic Lupus Erythematosus (SLE) (systemic autoimmune inflammation that may contribute to persistent ENT symptoms in some people) [2]
Real-world example (pattern, not a diagnosis): someone may report “three sinus infections in six months” treated with antibiotics, yet the congestion and facial pressure never fully clear—and they also notice nose crusting or nosebleeds. That combination is one reason clinicians consider non-infectious causes.
If usual allergy or infection treatments aren’t working, consider whether immune-driven inflammation could be part of the picture.

What Is Sinus Inflammation (and What Makes It “Chronic”)?
Acute vs. chronic inflammation (simple definition)
- Acute sinus inflammation is short-term swelling—often tied to a viral cold—and usually improves over days to a couple of weeks.
- Chronic sinus inflammation generally means symptoms lasting more than 12 weeks, or symptoms that recur frequently over an extended period.
If you want a deeper explainer on timelines, symptoms, and common causes, see our chronic sinusitis overview: https://sleepandsinuscenters.com/chronic-sinusitis
Why chronic inflammation matters
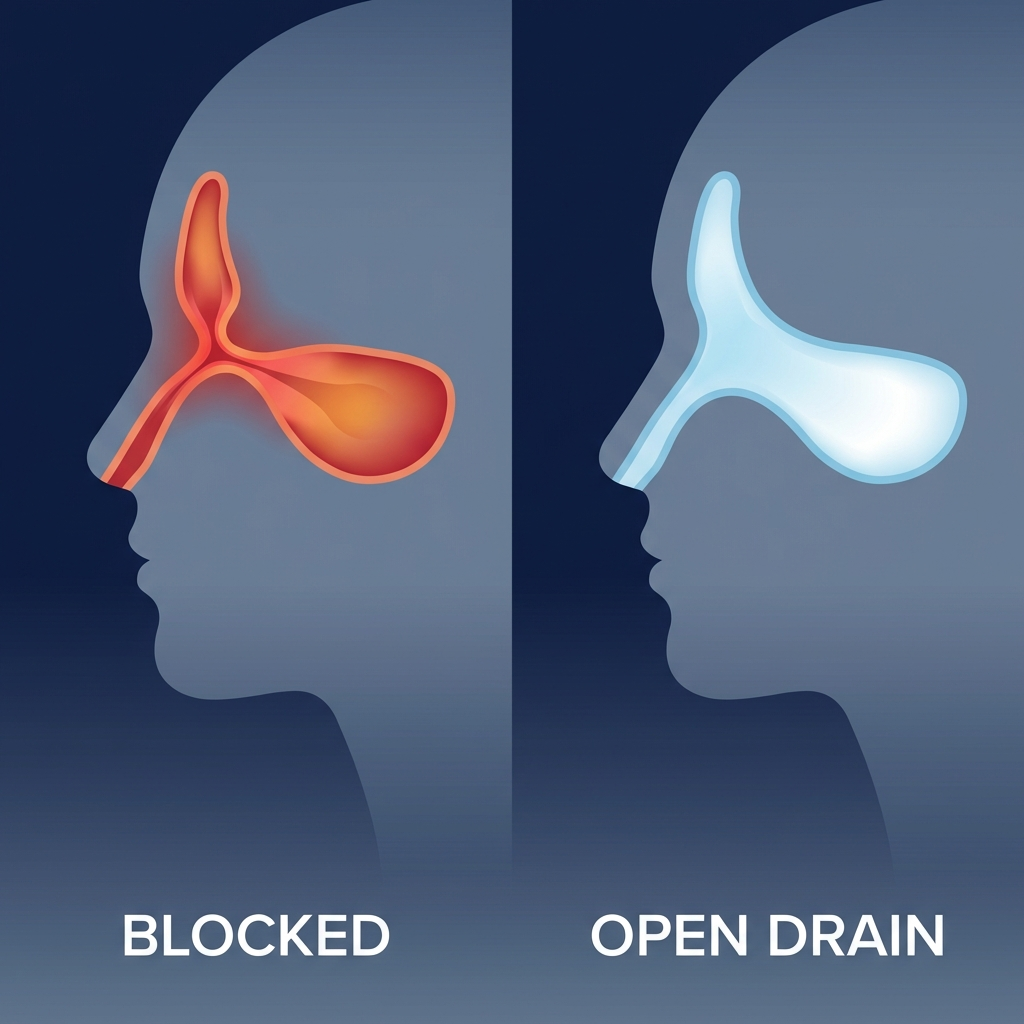
When swelling persists, it can block normal drainage and airflow. Over time, that can contribute to facial pressure and a “full” feeling; impaired smell and taste; thick post-nasal drip; fatigue from poor sleep and constant inflammation; and in some inflammatory conditions, crusting, irritation, scarring, or nosebleeds. [1]
Another practical way to think about it: your sinuses are like small rooms with narrow doorways for ventilation and drainage. If the “doorways” stay swollen shut, mucus and inflammation can build up—sometimes inviting secondary infections even if infection wasn’t the original problem. [1]
Persistent swelling can block drainage, worsen symptoms, and sometimes invite secondary infections—even when infection wasn’t the original cause.

How Autoimmune Diseases Trigger Sinus & Nasal Inflammation
“Immune system misfire” in everyday terms
In autoimmune conditions, the immune system may mistakenly target structures in and around the nose, such as the nasal lining (mucosa), small blood vessels, and cartilage. The result can be persistent swelling—and in some cases, tissue irritation or damage that makes symptoms more severe or harder to treat than ordinary congestion.
How this can feel day to day
People often describe symptoms as “always there,” rather than coming and going with weather changes, a specific season, or a known exposure.
Inflammation pathways researchers are studying (simple, non-technical)
Chronic rhinosinusitis involves complex immune signaling. Research describes shared inflammatory “switches” between chronic rhinosinusitis and autoimmune disease, including Th-17–related pathways that can amplify ongoing inflammatory activity. [1]
The takeaway: in some people, the immune system’s settings may be “turned up,” making inflammation more likely to persist.
Why Autoimmune Sinus Inflammation May Feel Different From Allergies
Allergies often cause itching/sneezing and tend to fluctuate with seasons or exposure. Autoimmune sinus inflammation may be more persistent day-to-day, more painful or irritating, and more likely to include bleeding, crusting, or sores inside the nose. [2,3]
A brief office summary you may hear: when symptoms don’t match the usual allergy or infection pattern—especially when there’s crusting or bleeding—clinicians widen the differential.
Inflammation from autoimmune disease may be steadier, more irritating, and less responsive to typical allergy approaches.
Autoimmune Conditions Most Often Linked to Sinus Symptoms
This section is educational—not a way to self-diagnose. Similar symptoms can come from non-autoimmune causes, so persistent or unusual symptoms deserve a medical evaluation. Signs such as crusting, nosebleeds, or sores are uncommon in typical sinus infections and warrant further assessment.
Granulomatosis with Polyangiitis (GPA / Wegener’s)
GPA can affect the upper airway, including the nose and sinuses. Possible features include chronic congestion, sinus pressure, crusting, and nosebleeds. [3] Early recognition matters because this condition can also involve other organs (such as the lungs or kidneys). [3]
Red-flag cluster to take seriously: significant crusting + frequent nosebleeds + persistent congestion that doesn’t respond as expected, especially if paired with symptoms elsewhere in the body. Seek medical evaluation promptly. [3]
Example: recurrent bloody crusts when blowing the nose plus sinus pressure that persists despite multiple “sinus infection” treatments. That pattern doesn’t confirm GPA—but it’s a reason to ask about broader evaluation.
Sarcoidosis
Sarcoidosis can create inflammatory granulomas that may involve the nasal passages and sinuses, leading to chronic obstruction or recurring symptoms in some patients. [2]
People often assume sarcoidosis is “only a lung condition,” but it can involve multiple areas. If nasal blockage is persistent and unusual, clinicians may consider inflammatory conditions in the differential based on the full history and exam. [2]
Systemic Lupus Erythematosus (SLE)
SLE is a systemic autoimmune condition. Some people with lupus experience ENT symptoms that may overlap with inflammation or dryness, and sometimes recurrent infections or irritation can contribute to ongoing sinus complaints. [2]
In other words, lupus may not “look like sinusitis” in a straightforward way—so clinicians interpret nasal/sinus symptoms in the context of the whole health picture. [2]
Certain autoimmune diseases can directly involve the nose and sinuses, and early recognition is important when red flags are present.
Symptoms of Autoimmune-Related Sinus Inflammation
Common sinus symptoms (may overlap with other causes)
- Persistent congestion/stuffiness
- Post-nasal drip
- Facial pressure/pain
- Reduced smell/taste
- Recurrent “sinus infections”

Symptoms that are more suggestive of an autoimmune cause
- Severe crusting
- Frequent nosebleeds
- Ulceration/sores inside the nose
- Symptoms that do not improve with standard allergy treatments
- Ongoing symptoms despite repeated antibiotics (when infection isn’t the main driver) [2,4]
These signs are uncommon in typical sinus infections and warrant further medical assessment.
For a focused checklist, see: https://sleepandsinuscenters.com/blog/autoimmune-sinusitis-key-signs-your-sinus-problems-20260203051202 [4]
When sinus symptoms may indicate broader (systemic) illness
- Significant fatigue or unexplained fevers
- Joint pain or rash
- Shortness of breath or coughing blood (urgent)
- Kidney-related symptoms such as swelling or dark urine (urgent) [3]
If you’re unsure whether symptoms “count,” write a short timeline (when symptoms started, what helped, what didn’t, and any non-sinus symptoms). That kind of history is often useful clinically.
If your sinus symptoms persist and include crusting, bleeding, or symptoms outside the sinuses, seek medical evaluation.
Causes & Triggers: Autoimmune Inflammation vs. “Regular” Sinusitis
How autoimmune sinus inflammation differs from: allergies (triggered by allergens; often improves with avoidance and allergy-directed care); viral colds (usually self-limited); bacterial sinus infection (may follow a pattern where antibiotics are sometimes appropriate); structural blockage (deviated septum, polyps, or narrow drainage pathways can keep symptoms going).
Because symptoms can overlap, testing can be helpful. If allergy patterns are suspected, allergy testing can help clarify whether allergies are part of the picture: https://sleepandsinuscenters.com/allergy-testing
Why symptoms can become chronic
Autoimmune-driven inflammation can persist because the immune system remains activated. Over time, inflammation may contribute to tissue changes and poor drainage, which can increase the risk of secondary infections—even if infection wasn’t the original cause. [1]
When symptoms repeatedly return or never fully resolve, it’s time to reassess the root cause, not just treat each flare.
Diagnosis: How Doctors Evaluate Possible Autoimmune Sinusitis

Step 1 — ENT evaluation and history
A clinician maps how long symptoms have lasted, which treatments helped (or didn’t), whether there’s crusting, bleeding, or ulcers, and whether symptoms exist outside the nose/sinuses (skin, joints, lungs, kidneys).
Step 2 — Exam and in-office testing
A detailed nasal exam may be done, sometimes including nasal endoscopy to look deeper into the nasal passages. It can help identify inflammation patterns, drainage issues, crusting, polyps, or signs that suggest further workup. What to expect: https://sleepandsinuscenters.com/blog/what-is-nasal-endoscopy----and-is-it-painful
Step 3 — Imaging
A CT scan of the sinuses can show chronic swelling, blockage patterns, and structural contributors. Learn more: https://sleepandsinuscenters.com/blog/sinus-ct-scan-what-it-shows-and-how-it-helps-diagnose-sinus-issues
Step 4 — Lab work and referrals (when indicated)
If autoimmune disease is suspected, labs may be considered (examples: ANCA when certain vasculitis patterns are suspected; ANA as a general autoimmune screening tool). Positive results require careful clinical correlation and, when appropriate, confirmatory testing; these markers alone do not confirm autoimmune sinusitis. Coordination with relevant specialists is often recommended when systemic disease is a concern. [1,3]
A structured evaluation—history, targeted exam, imaging, and selective labs—helps clarify whether immune dysregulation is contributing to your symptoms.
Treatment Options for Autoimmune-Related Sinus Inflammation

Treatment generally has two goals: improve day-to-day symptoms and address underlying immune inflammation when present. The approach depends on the individual and the confirmed diagnosis.
At-home and supportive care
Supportive measures may help reduce irritation and crusting: saline rinses/irrigation to improve clearance; humidification and hydration; gentle moisturization when clinician-directed. [4]
Tip: Rinses are most helpful when they’re consistent and comfortable—not overly forceful. For safety, use sterile/distilled water (or properly boiled and cooled water), especially for irrigation.
Medications that reduce local inflammation
Local anti-inflammatory treatments can be used in many chronic sinus conditions: intranasal corticosteroid sprays; steroid rinses for select situations (when appropriate). For some people, these reduce swelling enough to improve airflow, drainage, and sleep—without repeated antibiotics.
Systemic treatments (when autoimmune disease is confirmed/suspected)
When a systemic autoimmune condition is driving symptoms, treatment may include short courses of oral steroids (individualized), immunosuppressive medications, or biologic therapies in select diseases. These should be used only under close medical supervision, as they can have significant side effects. [1,2]
Treating infections when they are truly present
Antibiotics can help when bacterial infection is suspected or confirmed. Repeated or prolonged antibiotics may not help if inflammation is autoimmune-driven—highlighting the need for thorough evaluation.
Procedures and surgery (when needed)
Procedures may be considered to improve airflow and drainage, address structural blockage, or obtain tissue/biopsy when indicated. If immune inflammation remains active, surgery is usually adjunctive—it supports symptom control but doesn’t replace medical management. [1,2]
Effective treatment often combines symptom relief with targeted therapy for the underlying immune process.
Lifestyle Tips to Reduce Sinus Flares (Autoimmune-Friendly and Practical)
Protect the nasal lining
- Use a humidifier in dry months (and clean it regularly)
- Avoid smoke/vaping and strong fragrances
Reduce irritation and promote drainage
- Keep a consistent saline rinse routine if it helps (use sterile/distilled or properly boiled-and-cooled water for safety)
- Warm showers or steam can provide comfort if tolerated [4]
Manage comorbid triggers
Autoimmune disease and allergies can coexist. If symptoms have a seasonal pattern, testing may help clarify contributors. Track possible irritants (dusty environments, smoke exposure, dry indoor heat) alongside medication changes—patterns can help tailor treatment. [1]
Small daily habits that protect the nasal lining and reduce irritation can make flares less frequent and more manageable.
When to See a Doctor (and When It’s Urgent)
Make an appointment if you have:
- Sinus symptoms lasting 12+ weeks
- Recurrent “sinus infections” that keep returning
- Symptoms that don’t respond to typical allergy approaches [2,4]
Seek urgent care/ER for:
- Heavy or recurrent nosebleeds you can’t stop
- Facial swelling with severe fever
- Vision changes, severe headache, or stiff neck
- Chest symptoms such as coughing blood or significant shortness of breath [3]
If symptoms are persistent, unusually severe, or paired with red flags, don’t wait—seek timely care.
FAQs
Can lupus cause chronic sinus problems?
Lupus is a systemic inflammatory condition and may contribute to persistent nasal/sinus symptoms in some people. Because many non-autoimmune problems can look similar, evaluation is important. [2]
What does autoimmune sinusitis feel like?
It’s often persistent and may include congestion and pressure like other sinus problems, but can be more associated with crusting, bleeding, or sores, and may respond poorly to standard allergy medications. This pattern is often described as autoimmune sinus inflammation. [2,4]
Is autoimmune-related sinus inflammation contagious?
No. Autoimmune inflammation is not contagious. However, secondary infections (if they occur) can be contagious depending on the specific infection.
Can allergies and autoimmune disease both be involved?
Yes. Inflammation can have more than one contributor, and researchers note overlap in immune pathways across conditions. [1]
What kind of doctor should I see first—ENT or rheumatology?
Many people start with an ENT evaluation to assess the nasal/sinus anatomy and inflammation directly. If symptoms, exam, imaging, or labs suggest systemic autoimmune disease, coordinated care and referral may be recommended. [3,4]
Conclusion: Treat the Symptoms—But Also Look for the Root Cause
Most chronic sinus symptoms are not autoimmune. But when congestion and pressure become long-lasting, unusually severe, or paired with crusting, bleeding, or ulcers, it’s worth evaluating for less common causes—including autoimmune sinus inflammation. These signs are uncommon in typical sinus infections and warrant further medical assessment.
A structured workup (history, nasal exam, possible endoscopy, imaging, and targeted labs when needed) can clarify what’s driving symptoms and help guide a treatment plan that addresses both comfort and root cause.
CTA: If you’re dealing with persistent or recurrent sinus symptoms—especially if they aren’t responding as expected—you can book an appointment to be evaluated at https://www.sleepandsinuscenters.com/. For personalized diagnosis and treatment, please consult your healthcare provider.
References
1. NIH/PMC (2024). Chronic rhinosinusitis immune pathways and autoimmune links (incl. Th-17). https://pmc.ncbi.nlm.nih.gov/articles/PMC11458559/
2. Top Doctors (2025). Nasal inflammation/blockage in autoimmune diseases: causes, symptoms, treatment. https://www.topdoctors.co.uk/medical-articles/understanding-nasal-inflammation-and-blockage-in-autoimmune-diseases-causes-symptoms-and-treatment-options/
3. Johns Hopkins Medicine (2024). Granulomatosis with polyangiitis (Wegener’s). https://www.hopkinsmedicine.org/health/conditions-and-diseases/wegeners-granulomatosis
4. Sleep & Sinus Centers (2026). Autoimmune sinusitis: key signs. https://sleepandsinuscenters.com/blog/autoimmune-sinusitis-key-signs-your-sinus-problems-20260203051202
Final disclaimer: This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.