Chronic Sinusitis and Autoimmune Disease Connection: Causes, Symptoms, and Treatment
Chronic sinus symptoms can be frustrating—especially when they keep coming back despite “doing all the right things.” For many people, chronic rhinosinusitis is local inflammation limited to the nose and sinuses. But in some cases, ongoing sinus inflammation may reflect a bigger immune pattern happening elsewhere in the body. Researchers have increasingly explored the chronic sinusitis and autoimmune disease connection, finding meaningful associations and shared biology; however, current evidence shows correlation, not proven cause-and-effect for all patients. [1], [4]
Chronic sinusitis, also called chronic rhinosinusitis (CRS), is long-lasting inflammation of the nose and sinus lining. Autoimmune disease refers to conditions where the immune system mistakenly attacks the body’s own tissues. CRS does not automatically mean you have an autoimmune condition—and having an autoimmune condition doesn’t guarantee chronic sinusitis—but studies suggest there can be overlap in certain patients. [1], [4]
If you’re looking for a deeper overview of symptoms and care options, see our page on chronic sinusitis at Sleep and Sinus Centers of Georgia: https://sleepandsinuscenters.com/chronic-sinusitis
What Is Chronic Sinusitis (Chronic Rhinosinusitis)?
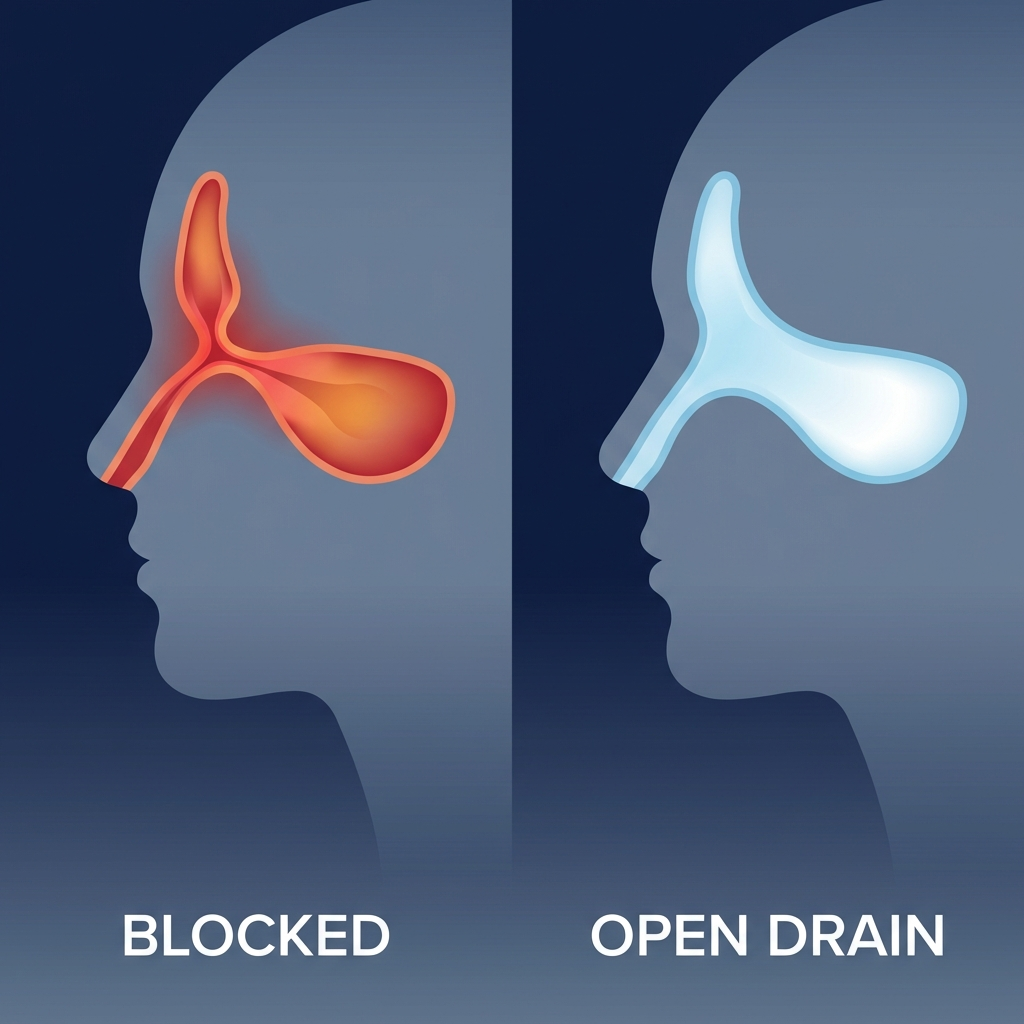
CRS is typically defined as sinus inflammation lasting 12 weeks or longer, often with ups and downs in symptoms. It’s not just “a lingering cold”—it’s an ongoing inflammatory condition that can affect breathing, sleep, energy, and quality of life.
If you’re unsure where you fall, this guide on acute vs. chronic sinusitis breaks down key differences: https://sleepandsinuscenters.com/blog/acute-vs-chronic-sinusitis-key-differences-and-treatment-options
Common CRS symptoms (what patients feel day-to-day)
- Nasal congestion or a blocked nose
- Thick drainage or post-nasal drip
- Facial pressure/pain
- Reduced sense of smell (and taste)
- Fatigue and poor sleep quality
Many patients describe it less like “being sick” and more like a persistent baseline: “My nose never fully clears, and I wake up tired even when I sleep.”

CRS with nasal polyps vs. CRS without nasal polyps (why it matters)
CRS is often discussed in two main subtypes:
- CRS with nasal polyps (CRSwNP)
- CRS without nasal polyps (CRSsNP)
Nasal polyps are soft, noncancerous growths that develop from chronically inflamed tissue. They can worsen congestion, reduce smell, and contribute to more persistent symptoms. This distinction matters because polyp-related CRS often reflects a stronger inflammatory component and may lead to different treatment pathways, sometimes including biologic medications approved for nasal polyps or surgery. [8], [9]
To learn more, read our post on nasal polyps and how they relate to chronic inflammation: https://sleepandsinuscenters.com/blog/what-are-nasal-polyps
Bottom line: CRS is a long-standing inflammatory condition that can significantly impact daily life, and identifying the subtype helps guide care.

What Are Autoimmune Diseases? (Quick, Clear Overview)
Autoimmune diseases involve immune dysregulation—an imbalance where the immune system’s “threat detection” becomes misdirected or overly active, leading to inflammation that can affect joints, glands, skin, nerves, or other organs.
A helpful analogy: the immune system normally works like a smoke alarm—loud when there’s real danger, quiet when the danger is gone. In autoimmune disease, that alarm may keep blaring or go off when there’s no “fire,” driving ongoing inflammation.
Examples of autoimmune diseases often discussed alongside CRS research
- Rheumatoid arthritis (RA)
- Systemic lupus erythematosus (SLE)
- Sjögren’s disease
- Multiple sclerosis (MS)
- Autoimmune thyroid disease (including Hashimoto’s-related hypothyroidism)
- Type 1 diabetes [3], [4]
Immune “dysregulation” in plain language
- Stay activated too long
- React too strongly
- Confuse the body’s tissues for a threat
Key idea: Autoimmune conditions reflect an overactive or misdirected immune response, which may overlap with chronic inflammation in the sinuses for some people.
The Evidence — What Research Says About the Connection
When people search for the chronic sinusitis and autoimmune disease connection, they’re often asking: “Are these conditions related?” Research increasingly suggests they can be—through shared genetics, shared inflammatory pathways, and higher rates of certain diagnoses occurring together. Association, however, does not prove causation. [3], [4]
Shared genetic risk between CRS and autoimmune diseases
Large-scale analyses suggest a genetic correlation between CRS and multiple autoimmune conditions, including RA, hypothyroidism, type 1 diabetes, MS, and SLE. [3], [4] Some individuals may inherit immune-related “wiring” that increases susceptibility to chronic inflammation across more than one body system—suggesting overlapping biological pathways regulating inflammation and immune response.
Sinusitis history linked to higher risk of rheumatic disease
A history of sinusitis may be associated with a higher incidence of certain rheumatic diseases—such as Sjögren’s disease and antiphospholipid syndrome. [4] One summary reported roughly a 40% higher relative risk in some populations. [7] This reflects correlation seen in observational data and does not establish that sinusitis causes rheumatic disease.
What this DOES and DOES NOT prove
Does: support awareness, appropriate screening conversations, and coordinated care when symptoms extend beyond the sinuses.
Does not: prove CRS causes autoimmune disease (or vice versa) for every person. Association is not the same as certainty.
A practical takeaway: if CRS is unusually persistent, severe, or accompanied by systemic symptoms, it’s reasonable to widen the diagnostic lens.

Why Might They Be Linked? (Mechanisms Explained Simply)
Shared genetic pathways (your “inflammation wiring”)
Some gene pathways regulate how strongly the immune system reacts and how quickly inflammation resolves. If those pathways tilt toward persistent activation, a person may be more prone to chronic inflammatory conditions—whether in the sinuses, joints, or glands. [3], [4]
Molecular mimicry (when the immune system gets “confused”)
Immune responses to microbes may accidentally cross-react with the body’s own tissues in genetically susceptible people. This broader autoimmune concept may be relevant to chronic airway inflammation but remains a hypothesis. [1], [4]
Th17 inflammation and chronic immune activation
Th17-related signaling is linked to persistent inflammation and appears in multiple autoimmune diseases and in some CRS patterns, helping explain hard-to-control inflammation. [4]
Inflammatory mediators and proteins being studied (future diagnostic clues)
Proteins such as IL-10, CXCL10, and CD6 are being investigated for how they may connect CRS subtypes with systemic immune signals. [2], [6]
Emerging science points to shared immune pathways in a subset of patients, helping explain why sinus and systemic inflammation can overlap.
Symptoms — How to Tell If CRS Might Be “Autoimmune-Associated”
CRS symptoms that can overlap with systemic inflammation
- Persistent or frequently recurring CRS symptoms despite guideline-based care
- Fatigue or “brain fog” that feels disproportionate to nasal symptoms alone
- Flares that seem to involve multiple body systems at once
A common pattern is “stacking” symptoms—sinuses flare, then joints ache, then exhaustion hits. That pattern doesn’t confirm autoimmunity, but it’s often why clinicians consider additional history, labs, or referral.
Red flags suggesting you should ask about autoimmune evaluation
- Dry eyes or dry mouth (Sjögren’s pattern)
- Joint pain, swelling, or morning stiffness (RA pattern)
- Rashes, mouth ulcers, or unexplained fevers (lupus-type clues)
- Numbness/tingling or neurologic symptoms (MS-type clues)
- Thyroid-type symptoms (cold intolerance, constipation, hair loss, weight changes)
When symptoms are urgent (seek prompt care)
- High fever, severe headache, swelling around the eye, or vision changes
- Stiff neck, confusion
- New neurologic deficits
If sinus flares coincide with broader systemic symptoms or red flags, ask your clinician whether autoimmune screening is appropriate.
Who Is Most at Risk?
Risk factors that may increase suspicion of a CRS–autoimmune overlap
- Personal history of autoimmune disease
- Strong family history of autoimmune disease
- CRS with nasal polyps or severe inflammation requiring repeated steroid courses or multiple interventions [8], [9]
Why severity can matter (including likelihood of surgery)
Chronic sinusitis—particularly with nasal polyps—can be associated with a higher likelihood of needing sinus surgery in some patients, reflecting how persistent inflammation can remodel sinus tissue over time. [9], [10]
The more persistent and severe the inflammation, the more important it becomes to consider overlapping contributors—including possible autoimmune conditions.
Diagnosis — What to Expect at an ENT Visit (and When Rheumatology Helps)
ENT evaluation for chronic sinusitis
- Detailed symptom history (timing, triggers, exposures)
- Nasal exam and/or endoscopy
- CT imaging when needed to confirm objective inflammation and map anatomy
Clues that may prompt broader workup
- CRS that doesn’t improve with evidence-based therapy
- Frequent relapse after stopping steroids
- Systemic symptoms (joint pain, dryness, rashes, unexplained fatigue)
Possible labs your clinician may consider (case-dependent)
- Autoantibodies (e.g., ANA, RF/anti-CCP, SSA/SSB)
- Inflammatory markers
- Thyroid labs
Objective sinus findings plus a careful review of systemic symptoms help determine when to involve rheumatology or additional testing.
Treatment — Managing CRS When Autoimmune Disease Is Part of the Picture
The goal is usually to reduce inflammation, improve drainage, and address contributing factors—while also considering how systemic immune conditions and medications may influence symptoms.
Standard chronic sinusitis treatments (foundation of care)
- Daily saline irrigation
- Intranasal steroid sprays (or steroid rinses when prescribed)
- Short courses of antibiotics only when bacterial infection is suspected
- Oral steroids may be used for severe flares, weighing potential benefits and risks; because systemic steroids can have side effects (e.g., mood changes, blood sugar elevation, bone effects), they are used thoughtfully and typically for limited durations

Treating contributing conditions (often overlooked)
- Allergic rhinitis (which may be clarified through allergy testing: https://sleepandsinuscenters.com/allergy-testing)
- Asthma or aspirin-exacerbated respiratory disease (AERD), when present
- Reflux, irritant exposure, and indoor air quality issues
When procedures or surgery may be recommended
When inflammation and blockage persist, options may include balloon procedures or endoscopic sinus surgery to improve ventilation and drainage—particularly for patients with nasal polyps or high disease burden. In appropriate patients with CRSwNP, biologic therapies approved for nasal polyps may reduce polyp size, improve symptoms, and lower the need for systemic steroids or repeat surgery. [9]

Coordinated care: ENT + rheumatology/immunology
- Systemic inflammation may influence sinus inflammation
- Immune-modulating medications can affect infection risk and treatment choices
- Aligning ENT and autoimmune care plans can reduce conflicting approaches
Most patients improve with consistent, guideline-based care; when autoimmunity is involved, coordination across specialties helps tailor a safer, more effective plan.
Lifestyle Tips to Support Sinus and Immune Health (Patient-Friendly)
Daily habits that help many CRS patients
- Consistent saline rinses using safe technique
- Sleep support (address congestion, consider head elevation)
- Hydration and careful humidification (avoiding overly humid indoor air)
If you rinse, use sterile/distilled water (or water that has been boiled and cooled) and keep bottles clean—small technique details can make a big difference in comfort and safety.
Trigger reduction (especially if the immune system is “primed”)
- Avoid smoke and vaping exposure
- Minimize strong fragrances and harsh cleaning chemicals
- Reduce dampness/mold risk; consider HEPA filtration in sleeping areas
Self-monitoring: track patterns that help your clinician
- Symptom diary and likely triggers
- Response patterns (e.g., antihistamines vs. steroids)
- New systemic symptoms (joints, skin, dryness)
Simple, consistent habits plus tracking your patterns can meaningfully support your care plan over time.
FAQs (For Featured Snippets)
Can chronic sinusitis cause autoimmune disease?
Current research supports an association but does not prove that chronic sinusitis causes autoimmune disease. [4], [7]
Which autoimmune diseases are most linked with chronic sinusitis?
Research highlights genetic correlation/associations with RA, autoimmune thyroid disease, type 1 diabetes, MS, SLE, and rheumatic diseases like Sjögren’s in some studies. [3], [4]
If I have an autoimmune disease, will I need sinus surgery?
Not necessarily. Surgery depends on anatomy, inflammation severity, nasal polyps, and how symptoms respond to medical therapy. [9]
What symptoms suggest my sinus issues might be autoimmune-related?
CRS plus systemic signs—dry eyes/mouth, joint swelling/stiffness, rashes, unexplained fatigue—may warrant a discussion about evaluation.
Should I see an ENT or a rheumatologist first?
If sinus symptoms are the main issue, many people start with ENT. If systemic symptoms are prominent, co-management may be useful.
Key message: Associations exist, but personalized evaluation is essential to determine the right next steps.
Conclusion — What to Do Next
The chronic sinusitis and autoimmune disease connection is an active area of research. The key takeaway is that chronic sinus inflammation and autoimmune disease can share genetic and immune pathways—and that matters most when symptoms are persistent, severe, or involve multiple body systems. [3], [4]
If you’re dealing with ongoing sinus symptoms, consider scheduling an evaluation with Sleep and Sinus Centers of Georgia and bringing a brief timeline of your symptoms, past treatments, and any non-sinus symptoms (like joint issues, dryness, rashes, or fatigue). A comprehensive workup can help clarify what’s driving inflammation and what next steps may fit your situation.
Ready to get answers? Book an appointment here: https://www.sleepandsinuscenters.com/
Next step: If symptoms persist or broaden beyond the sinuses, a coordinated ENT–rheumatology approach can help you move forward with confidence.
References
1. https://pmc.ncbi.nlm.nih.gov/articles/PMC11458559/
2. https://pmc.ncbi.nlm.nih.gov/articles/PMC12750445/
3. https://www.nature.com/articles/s41598-020-75815-x
4. https://rmdopen.bmj.com/content/10/1/e003622
5. https://www.jacionline.org/article/S0091-6749(25)00210-6/fulltext
6. https://pmc.ncbi.nlm.nih.gov/articles/PMC11299433/
7. https://bmjgroup.com/sinusitis-linked-to-40-heightened-risk-of-rheumatic-disease/
8. https://int.livhospital.com/chronic-sinus-infection-autoimmune-disease/
9. https://onlinelibrary.wiley.com/doi/10.1002/lio2.70340
10. https://www.medpagetoday.com/rheumatology/generalrheumatology/108916
Disclaimer
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.