Sinus Pressure Without Congestion: Causes, Symptoms, and When to See a Doctor
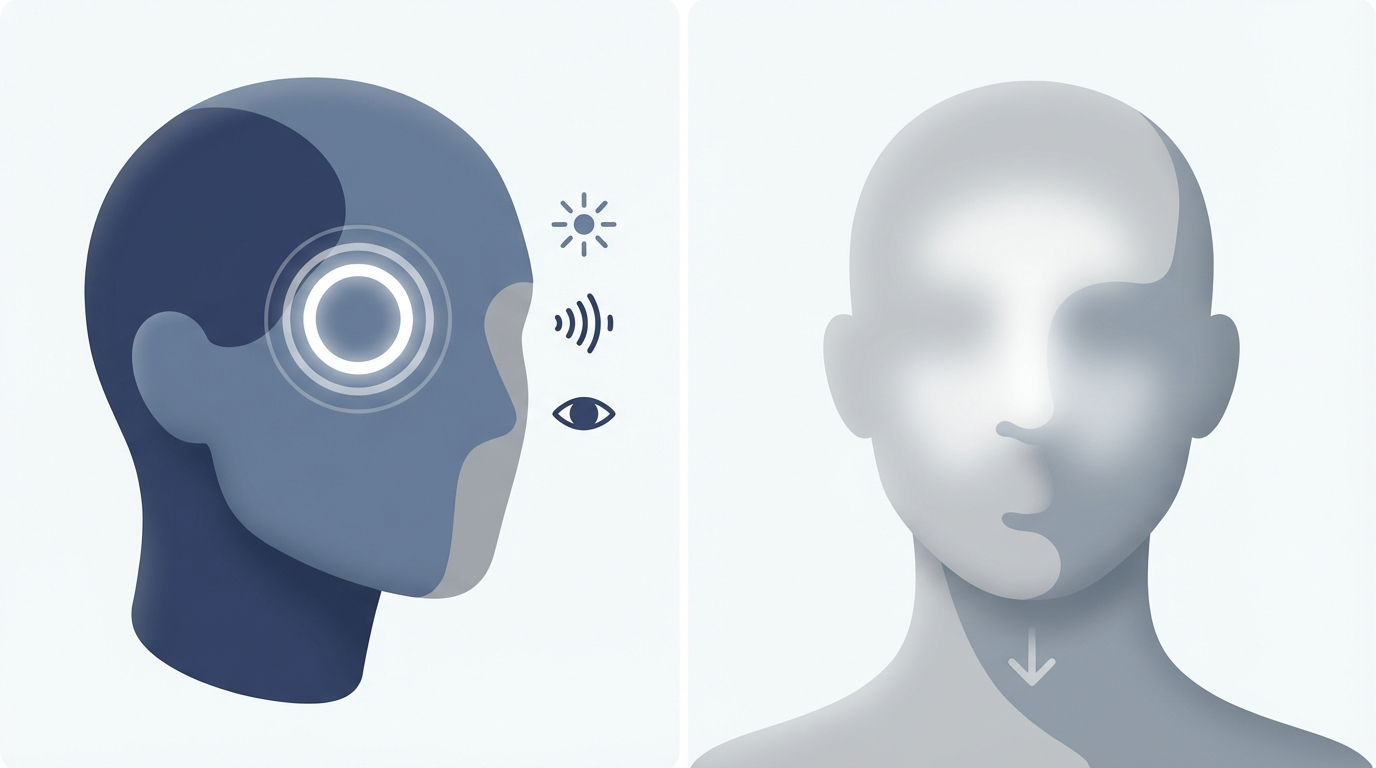
Feeling pressure in your forehead, cheeks, or around your eyes usually makes people think “sinus problem.” But sinus pressure without congestion is common—and it doesn’t always mean your sinuses are blocked or infected. In many cases, facial pressure comes from a headache disorder (especially migraine) or inflammation that doesn’t create a very stuffy nose.
Think of it this way: the “sinus area” is also where several sensitive nerves, muscles, and joints (including the jaw) can refer pain. So even when your nasal passages feel open, the sensation can still register as deep facial pressure.
Important note: “Sinus headache” is a controversial term. True sinus headaches from infection or blockage are relatively uncommon compared with migraine and other primary headache disorders.
Medical disclaimer: This article is for education only and isn’t a diagnosis or a substitute for medical care. If symptoms are severe, worsening, or unusual for you, seek medical evaluation.
Below is an educational guide to what this sensation can mean, what patterns to watch for, and when it’s time to get evaluated so you can pursue the right treatment.
Quick answer—can you have sinus pressure without congestion?
Yes. You can feel “sinus pressure” even when your nose is clear. That’s because the pressure sensation in the face can come from multiple sources—sinus lining irritation, nerve sensitivity, muscle tension, jaw issues, or headache disorders.
A big reason this is confusing: many people label any pain in the forehead/cheeks as a sinus headache without congestion, but migraine is a frequent cause of facial pressure even when there’s little to no nasal blockage. For example, you might feel pressure behind one eye, assume it’s sinus-related, and later notice it’s paired with light sensitivity or nausea—classic migraine clues.
If you’ve ever wondered whether you’re dealing with migraine vs sinus headache, this is a great place to start: https://sleepandsinuscenters.com/blog/migraine-vs-sinus-headache-key-differences-and-symptoms-explained.
Why this gets misdiagnosed so often
Symptoms overlap: forehead pressure, cheek aching, and pain around the eyes can show up in both sinus inflammation and headache disorders. Assumptions are easy: facial pain is widely associated with “sinus infection,” even when the nose is clear. Treatment depends on the cause: decongestants and antibiotics won’t help migraine, while migraine-specific care won’t address chronic nasal inflammation.
Summary: You can feel “sinus-area” pressure without a stuffy nose, and migraine is a common reason why.
What sinus pressure without congestion feels like (symptoms)
People describe sinus pressure without congestion in a few classic ways. The key is not just where it hurts, but how it behaves and what other symptoms come along with it.
Common symptoms
Common symptoms include: pressure or aching in the forehead, cheeks, bridge of the nose, or around/behind the eyes; a headache that feels full, tight, heavy, or pushing; facial tenderness (especially with touch); ear pressure, popping, or a “plugged” feeling that can happen alongside facial pressure. Some people also describe a mask-like heaviness across the mid-face—almost as if the cheeks and brow are subtly bruised, even when nothing is visibly swollen.
Symptoms that suggest a headache condition instead of a sinus problem
These features tend to align more with migraine (or another primary headache disorder) than with a true sinus blockage: throbbing pain or one-sided pain; nausea and/or vomiting; light or sound sensitivity; head pain that worsens with activity or exertion; aura (visual disturbances or changes) in some cases.
Symptoms that suggest sinus inflammation (even if you’re not “stuffed”)
Sinus-related inflammation can still be present without obvious congestion. Clues may include: post-nasal drip (mucus sensation in the throat); reduced sense of smell; symptoms that linger weeks to months, which may suggest chronic rhinosinusitis rather than a short-term viral illness. If you’re noticing long-lasting symptoms, you may also want to read about chronic sinusitis: https://sleepandsinuscenters.com/chronic-sinusitis.
Summary: Pay attention to what travels with the pressure—nausea and light sensitivity point to migraine, while smell changes and post-nasal drip point to sinus inflammation.

Causes of sinus pressure without congestion
There isn’t one single explanation for facial pressure without a stuffy nose. Here are the most common possibilities—starting with the ones that are often overlooked.
1) Migraine (the most common “sinus pressure” impostor)
Migraine can affect nerves in and around the face, creating pressure sensations in the forehead, cheeks, and behind the eyes. Some episodes don’t look like a “classic migraine,” which is why people may only notice facial pressure and assume it’s sinus-related. Sinus pressure without congestion can be a migraine presentation—especially when symptoms come and go, are triggered by light/sleep changes/stress, or are associated with nausea or sensitivity to sound.
2) Tension-type headaches (tight, band-like pressure)
Tension-type headaches often feel like tightness across the forehead and temples. That band-like pressure can be perceived as sinus pressure—particularly if you also have neck stiffness, stress, long screen time, or posture strain. Jaw clenching and muscle tension can amplify the sensation around the eyes and cheeks.
3) Cluster headaches (severe, one-sided pain around the eye)
Cluster headaches can cause intense, stabbing or drilling pain around one eye with eye/nose symptoms on the same side (watering eye, runny nose, eyelid droop). Because treatment differs from sinus care, recurring one-sided attacks warrant medical evaluation.
4) Allergies or nonallergic rhinitis (inflammation without major mucus buildup)
Allergic or irritant-triggered inflammation can swell the nasal lining and create facial pressure even when mucus and congestion aren’t dramatic. Triggers may include seasonal pollen, dust, pet dander, smoke, strong odors, or changes in indoor humidity. Learn more about testing: https://sleepandsinuscenters.com/allergy-testing.
5) Chronic rhinosinusitis (pressure can occur even without a “runny nose”)
Ongoing inflammation in the nose and sinuses can cause facial pressure, fatigue, and smell changes. Congestion may be mild, intermittent, or simply not the symptom you notice most.
6) Structural/nasal anatomy issues (airflow and drainage problems)
Anatomy differences—such as a deviated septum—may contribute to a sense of pressure or imbalance, sometimes worse on one side. If one-sided symptoms are a consistent theme, this overview may help: https://sleepandsinuscenters.com/deviated-septum-relief.
7) Barometric pressure or environmental pressure changes
Weather shifts, storms, altitude changes, flying, and diving can trigger facial pressure or headaches. For some people, these changes overlap with migraine triggers.
8) TMJ disorder (jaw joint dysfunction) and muscle tension
TMJ problems can refer pain into the temples, cheeks, and around the eyes—creating facial pressure without a stuffy nose. Clues can include jaw clicking, soreness with chewing, morning tightness, or a history of clenching/grinding.
9) Dental causes (tooth infection or inflammation)
Upper tooth problems can refer pain into the cheek and maxillary sinus region. Consider this possibility if there’s tooth sensitivity, pain with chewing, gum tenderness, swelling, or fever.
Summary: Many different problems can feel like “sinus pressure”—migraine is common, but inflammation, anatomy, jaw, and dental issues can all play a role.

How to tell if it’s sinus-related or a migraine/headache issue
The goal isn’t to self-diagnose—it’s to notice patterns that can guide a more accurate evaluation.
Symptom pattern clues
More suggestive of migraine or another headache disorder: throbbing or pulsing, possibly one-sided; nausea, light/sound sensitivity, worse with activity; episodic attacks with potential triggers (sleep changes, stress, weather); decongestants or antibiotics typically not helpful.
More suggestive of sinus inflammation: pressure/aching that may feel deep or full; post-nasal drip, reduced sense of smell, thick drainage; persistent symptoms over days to weeks; may improve with saline and anti-inflammatory nasal therapy.
The “bend forward test”—helpful but not definitive
More pressure on bending forward can happen with sinus inflammation, but it can also occur with other headache conditions. If bending reliably worsens symptoms—and episodes keep returning—track that pattern and share it at your visit. Persistent or severe symptoms should be evaluated regardless.
Summary: Track patterns over time—what else you feel and what helps—then share that snapshot with your clinician.
At-home relief and lifestyle tips (what you can try first)
For mild or occasional symptoms, conservative measures may help. If symptoms are frequent, severe, or escalating, self-treatment has limits—especially when the root cause is migraine, TMJ, or a dental problem.
Gentle home strategies for pressure relief
Warm compresses over the forehead/cheeks; hydration and a humidifier during dry seasons; saline spray or saline rinse to soothe irritation (when appropriate and tolerated); rest in a dark, quiet room if migraine features appear.
Trigger management (especially if migraine or tension is suspected)
Keep sleep and wake times consistent; don’t skip meals and stay hydrated; reduce screen glare/brightness if it worsens headaches; build short posture breaks into the day with neck/shoulder stretching and jaw relaxation.
Environmental steps if allergies are possible
Track high pollen or mold days and note symptom patterns; shower after outdoor exposure and consider changing clothes; maintain filtration/cleaning routines, especially in bedrooms; discuss over-the-counter options with a clinician to match your pattern.
Summary: Simple comfort measures can help, but frequent or severe episodes deserve a tailored plan.

Treatment options (based on the underlying cause)
Because sinus pressure without congestion can come from very different conditions, the best treatment depends on a correct diagnosis.
If migraine is the cause
Over-the-counter pain relievers help some; others need migraine-specific rescue options. Preventive strategies may be considered if attacks are frequent. Trigger identification and lifestyle adjustments can reduce episodes. Note: Decongestants and antibiotics do not treat migraine-related pressure.
If tension headache is the cause
Use heat/ice and gentle neck/shoulder stretching; make ergonomic adjustments and take regular movement breaks; address jaw clenching or sleep-related grinding when relevant.
If allergies/rhinitis or chronic rhinosinusitis is the cause
Use consistent saline irrigation and anti-inflammatory nasal therapy as guided by a clinician; evaluate for allergy triggers and consider targeted treatment if symptoms recur; consider further assessment if symptoms are persistent, seasonal, or impacting sleep. Learn more: chronic sinusitis (https://sleepandsinuscenters.com/chronic-sinusitis) and allergy testing (https://sleepandsinuscenters.com/allergy-testing).
If anatomy/structural issues contribute (like a deviated septum)
Medical management is often tried first. If symptoms persist, an ENT evaluation can clarify whether anatomy plays a major role and what options make sense: https://sleepandsinuscenters.com/deviated-septum-relief.
If TMJ is suspected
Use a soft diet during flares, apply heat, and practice jaw relaxation habits; seek dental/TMJ evaluation; consider a night guard if clenching/grinding is part of the pattern.
If dental infection is suspected
Seek dental evaluation promptly; untreated infection can worsen and spread.
Summary: The right treatment flows from the right diagnosis—what helps migraine won’t fix chronic sinus inflammation, and vice versa.
When to see a doctor (and when it’s urgent)
Knowing when to see a doctor for sinus pressure can prevent weeks of trial-and-error and help you get targeted relief.
Make an appointment soon if
Pressure/headache keeps returning or lasts more than 7–10 days without improvement; you get frequent “sinus headaches” but little congestion (possible migraine); symptoms interfere with sleep, work, or daily routines; you suspect allergies, chronic sinusitis, TMJ, or dental causes.
Seek urgent care/ER now for red flags
Sudden, severe “worst headache” you’ve ever had; new neurologic symptoms (weakness, confusion, fainting, speech trouble); high fever, stiff neck, significant swelling around an eye, or vision changes; facial swelling with significant dental pain or spreading redness.
Summary: Don’t wait on red flags—urgent symptoms need immediate evaluation.

What to expect at an ENT or medical visit (diagnosis)
A focused evaluation usually starts with your symptom story and patterns, then adds an exam and targeted testing if needed.
History and symptom pattern questions
You may be asked about duration, location, severity, and timing of symptoms; triggers such as weather, stress, sleep disruption, foods, and screens; migraine features like nausea and light sensitivity; allergy exposure, reflux symptoms, jaw clenching, and dental symptoms. Tip: Bring a short list of what you’ve tried (saline, antihistamines, pain relievers) and whether it helped “a lot,” “a little,” or “not at all.”
Possible exams/tests
Depending on the situation, the visit may include a nasal exam (sometimes with nasal endoscopy); allergy evaluation when triggers are suspected; imaging such as CT when chronic sinusitis or anatomy concerns are on the table.
Summary: Clear symptom notes plus a focused exam help your clinician match treatment to the true cause.
FAQs
Can you have a sinus infection without congestion?
Sometimes, but many cases described as “sinus headache without congestion” turn out to be migraine or another headache disorder. If symptoms recur and congestion is minimal, it’s reasonable to ask whether migraine is being missed. For more on chronic sinus symptoms, see: https://sleepandsinuscenters.com/chronic-sinusitis.
Why do my cheeks/eyes feel pressure but my nose is clear?
This can happen with migraine-related nerve sensitivity, allergies/rhinitis inflammation, TMJ dysfunction, dental issues, or barometric pressure changes.
Is sinus pressure without congestion usually migraine?
Migraine is a very common explanation for recurring facial pressure—especially when nausea, light sensitivity, throbbing, or activity-related worsening is present. Compare features here: https://sleepandsinuscenters.com/blog/migraine-vs-sinus-headache-key-differences-and-symptoms-explained.
Can weather/air pressure changes cause sinus pressure without congestion?
Yes. Barometric shifts can trigger facial pressure and headaches in some people, and may overlap with migraine susceptibility.
What’s the best OTC option for sinus pressure without congestion?
It depends on the cause (headache vs inflammation). Decongestants and antibiotics are not effective for migraine. If symptoms are frequent or you’re using OTC medications often, discuss safer long-term strategies with a clinician.
Summary: If OTC options aren’t helping—or you’re using them often—it’s time to get a tailored plan.
Key takeaways
Sinus pressure without congestion is common and not automatically a sinus infection. Migraine and other headache disorders are frequent causes of facial pressure. Allergies/inflammation, structural issues, pressure changes, TMJ, and dental problems can also contribute. If symptoms are recurring, lasting, or severe, an evaluation helps identify the cause and match the treatment to what’s actually happening.
If facial pressure keeps coming back—or you’ve been treating “sinus headaches” without much congestion—it may be time for a more targeted evaluation. To book an appointment, visit https://www.sleepandsinuscenters.com/.
References
1) https://www.medicalnewstoday.com/articles/sinus-headache-without-congestion
2) https://www.verywellhealth.com/sinus-headache-without-congestion-7500819
3) https://my.clevelandclinic.org/health/symptoms/24690-sinus-pressure
4) https://www.afcurgentcare.com/denver-park-hill/blog/sinus-pressure-without-congestion-what-you-need-to-know/
5) https://www.kaplansinusrelief.com/blog/sinus-pressure-no-congestion/
6) https://collincountyent.com/what-does-a-sinus-pressure-headache-feel-like/
Disclaimer
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.







