Chronic Sinusitis and Fatigue: How to Break the Cycle and Restore Energy
If you’ve been dealing with “sinus problems” for months and can’t figure out why you’re dragging through the day, you’re not imagining it. Chronic sinusitis is generally defined as sinus inflammation and symptoms lasting 12 weeks or longer, often including congestion, drainage, and facial pressure (Mayo Clinic). When symptoms don’t let up, fatigue can become one of the most disruptive parts of the condition—sometimes as burdensome as the pain and pressure themselves (The American Journal of Medicine).
This guide explains the link between chronic sinusitis and fatigue, how to recognize sinus-related exhaustion, why it happens, and a step-by-step way to improve energy by addressing sinus disease—from home care to medications to ENT procedures. If you want a deeper overview of symptoms and treatment options, you can also learn more about chronic sinusitis at Sleep and Sinus Centers of Georgia: https://sleepandsinuscenters.com/chronic-sinusitis
Can Chronic Sinusitis Really Make You Tired? (Yes—and It’s Common)
Chronic sinusitis isn’t “just a stuffy nose.” It’s a long-running inflammatory condition, and fatigue is a frequent complaint in people whose symptoms linger for months. In quality-of-life research, fatigue shows up as a major burden—sometimes rated as severely as facial pain or pressure (The American Journal of Medicine). In other words, it’s not a side note; for many people, it’s the symptom that breaks their routine.
The “tired but wired” pattern many sinus patients describe
- Daytime sleepiness (even after a full night in bed)
- Low motivation and reduced stamina
- “Brain fog” or trouble concentrating
- Feeling run-down during symptom flares
Fatigue can also show up alongside classic sinus symptoms—congestion, pressure, and thick drainage—making sinus-related tiredness feel like it comes in waves. Fatigue is a common associated symptom, not a diagnostic criterion on its own, and it has been reported as a meaningful indicator when sinus disease is active (Vanderbilt University Medical Center).
A common real-life example: you get through the workday, but by late afternoon you feel like your brain is buffering—words come slower, your patience is shorter, and even small tasks feel heavier than they should.
Why this fatigue is often underestimated
It’s easy to think “sinuses” only means facial pressure or a stuffy nose. But chronic sinusitis is an inflammatory condition (Cleveland Clinic), and inflammation plus poor sleep can affect the entire body—mood, focus, and energy included. That’s why chronic sinusitis tiredness can persist even when facial pain isn’t the main complaint.
A helpful way to think about it: sinusitis can act like a “background app” on your body—always running, always consuming resources—even when you’ve learned to tolerate the symptoms.
— Italic summary: Fatigue is a common, meaningful part of chronic sinusitis—not an afterthought. —
Symptoms — How to Tell If Your Fatigue May Be Sinus-Related
Common chronic sinusitis symptoms (with fatigue overlap)
Chronic sinusitis often includes (Mayo Clinic; Cleveland Clinic):
- Nasal congestion or obstruction
- Thick nasal drainage and/or post-nasal drip
- Facial pressure or pain
- Reduced sense of smell
- Cough or frequent throat clearing
- Fatigue and poor sleep, especially when congestion worsens at night
When people search for “nasal congestion sleep problems,” they’re often describing the same pattern: blocked breathing, restless nights, and low energy the next day. For example, you may fall asleep quickly but wake up repeatedly with a dry mouth from mouth-breathing, or you may wake earlier than usual because drainage triggers coughing. For a deeper dive on this link, explore how sinus issues affect sleep quality and ENT solutions: https://sleepandsinuscenters.com/blog/how-sinus-issues-affect-sleep-quality-and-ent-solutions
“Energy red flags” that suggest sinuses may be driving your exhaustion
Fatigue may be more sinus-related when you notice:
- You wake up unrefreshed even after adequate time in bed
- Your fatigue worsens with flares (weather changes, colds, allergens, indoor dust)
- Snoring or mouth breathing increases when congestion is worse
- Brain fog improves temporarily after a hot shower, clearing mucus, or rinsing the nose
That last point—brief relief after steam or a rinse—can be a helpful clue. It doesn’t prove the cause, but it suggests airflow and mucus burden may be part of why your energy tanks.
When fatigue may be from something else (but still worth evaluating)
Not all fatigue is sinus-related. Persistent exhaustion without sinus symptoms—or fatigue alongside issues like weight changes, palpitations, or symptoms of anemia or depression—deserves a broader conversation with a clinician. It’s also common for sinus problems to overlap with allergies or sleep-disordered breathing, so addressing one factor can make the overall picture easier to manage.
— Italic summary: If your energy dips track with nasal symptoms, your sinuses may be part of the story. —
Why Chronic Sinusitis Causes Fatigue (The Real Mechanisms)
1) Chronic inflammation drains energy
One major driver of chronic inflammation–related fatigue is the energetic cost of staying inflamed. When the body is stuck in a prolonged inflammatory response, you may feel run down, less resilient, and slower to recover after everyday stressors. Chronic sinusitis is widely described as an inflammatory condition (Mayo Clinic; Cleveland Clinic), which helps explain why energy can drop even when symptoms feel “familiar.”
If you’ve ever noticed that you “catch up on rest” but still feel depleted, ongoing inflammation can be part of that mismatch—your body may be working harder than you realize just to maintain baseline function.
2) Sleep disruption from congestion, pressure, and drainage
Sleep may be disrupted in several ways:
- Nasal blockage can lead to mouth breathing, snoring, and frequent micro-awakenings
- Post-nasal drip can trigger coughing or throat clearing at night
- Facial pressure can make it harder to fall or stay asleep
A practical example: you may not remember waking up, but your sleep can still be fragmented—like trying to charge your phone with a loose cable. You’re “plugged in” for eight hours, but the recharge is incomplete.
For a focused look at the sleep connection, see: https://sleepandsinuscenters.com/blog/how-sinus-issues-affect-sleep-quality-and-ent-solutions
3) Reduced airflow and “not breathing well at night”
Even without a formal sleep diagnosis, nightly nasal obstruction can make breathing feel less comfortable and less efficient. Over time, fragmented sleep can add up—especially if congestion is frequent or year-round. Many people describe this as waking up “already tired,” as if they never fully settled into deep, restorative sleep.
4) Immune system workload during recurring infections/flares
Some people experience repeated flare-ups. When your immune system keeps ramping up to deal with ongoing irritation or possible infections, fatigue can become part of the pattern.
Fatigue is commonly reported in chronic rhinosinusitis and can have a severe impact on quality of life, sometimes comparable to facial pain (The American Journal of Medicine).
— Italic summary: Treating inflammation and nighttime breathing often lifts energy. —

The Vicious Cycle — How Sinus Symptoms and Fatigue Keep Each Other Going
Step-by-step cycle (simple explanation)
A common loop looks like this:
1. Congestion/pressure/drainage → poorer sleep
2. Poor sleep → worse fatigue and lower daytime stamina
3. Fatigue → harder to keep consistent routines (hydration, home care, follow-ups)
4. Inflammation persists → symptoms continue
This cycle can feel especially discouraging because the thing that would normally help you recover—sleep—becomes less restorative right when you need it most.
Why “just resting more” often doesn’t fix it
Rest can help, but if nasal blockage and inflammation are the root issues, extra sleep time doesn’t always equal better sleep quality. That’s why treating the sinus component (not only the tiredness) can be pivotal for improving energy.
A simple way to test this idea: if you “sleep in” but still wake with heavy congestion, dry mouth, and brain fog, the issue may be sleep quality rather than sleep quantity.
— Italic summary: Breaking the loop starts with improving airflow and sleep quality. —
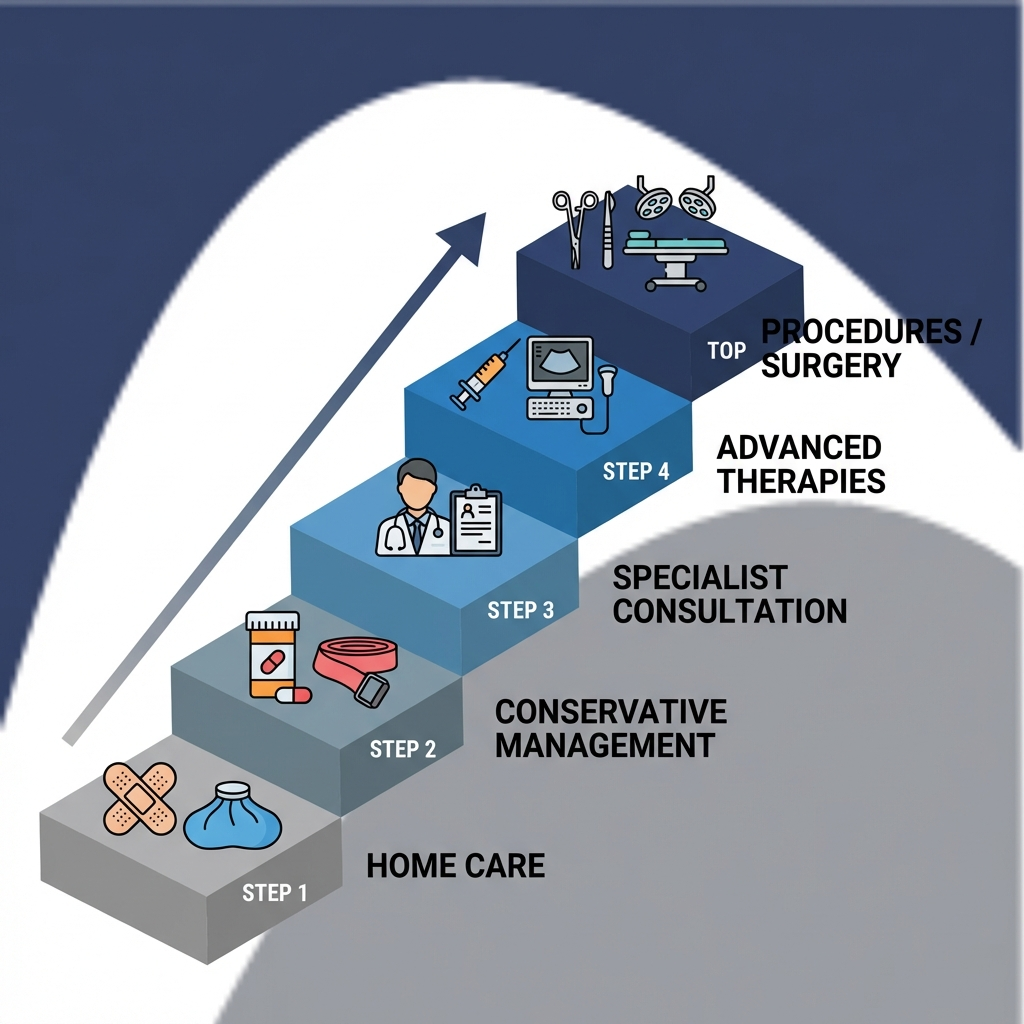
How to Break the Cycle: A Practical Treatment Ladder (Home → Medical → Procedures)

Step 1 — Daily at-home foundations (often overlooked but powerful)
These basics can support clearer nasal passages and reduce irritants:
- Nasal irrigation with saline to help flush mucus and particles and support drainage
- Important safety note: use distilled, sterile, or previously boiled-and-cooled water for rinses (Mayo Clinic guidance is commonly referenced).
- Humidification during dry seasons or in air-conditioned/heated indoor air
- Trigger reduction when possible (smoke, strong fragrances, heavy dust exposure)
Consistency matters here—many people do these steps only during “bad days,” even though regular routines may reduce flare frequency. If it helps, anchor the habit to a daily cue (for example, rinse after brushing your teeth in the evening, not only when you feel miserable).
Step 2 — Treat common drivers (allergies + inflammation)
Allergies can worsen swelling and congestion, fueling nighttime breathing problems and sinus fatigue. If symptoms are seasonal, triggered by pets, or worse indoors, it may be worth considering allergy testing to identify triggers: https://sleepandsinuscenters.com/allergy-testing
Depending on the situation, a clinician may discuss:
- Allergen avoidance strategies
- Non-sedating antihistamines (when appropriate)
- Anti-inflammatory nasal sprays
- Immunotherapy options for select patients
Even small changes—like reducing bedroom dust exposure—can matter because nighttime is when congestion has the biggest opportunity to disrupt sleep.
Step 3 — Medications your clinician may recommend
Medication choices depend on symptoms, exam findings, and history, but commonly discussed categories include:
- Nasal corticosteroid sprays to reduce inflammation
- Short courses of oral steroids in select cases of severe swelling (case-dependent)
- Antibiotics only when a bacterial infection is suspected—because not every flare is bacterial
A clear diagnosis helps target therapy. If you’ve tried “a little of everything” and still feel stuck, that’s often a sign it’s time for a more structured evaluation.
Step 4 — When anatomy or chronic blockage needs more than meds
If symptoms persist despite appropriate medical therapy, an ENT evaluation may look for factors such as:
- Narrow sinus drainage pathways
- Structural contributors to obstruction
- Persistent swelling and, in some cases, polyps
When airflow and drainage are chronically limited, inflammation can be harder to calm down—and fatigue can linger.
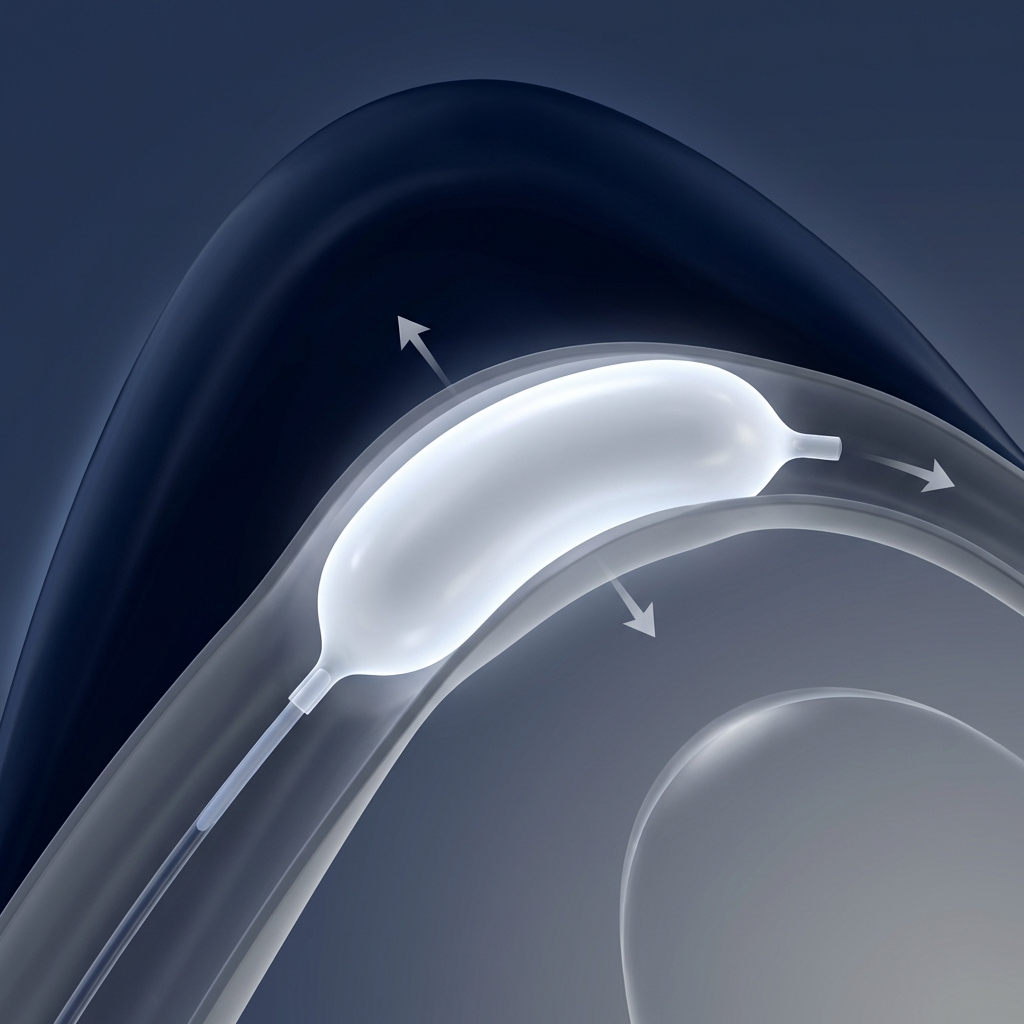
Step 5 — Minimally invasive procedures (when appropriate): Balloon Sinuplasty
For some patients who don’t improve with standard approaches, balloon sinuplasty may be an option: https://sleepandsinuscenters.com/balloon-sinuplasty
In simple terms, it’s a minimally invasive sinus procedure designed to widen drainage pathways, which can improve sinus ventilation and drainage. While outcomes vary between individuals, some patients experience improved nasal airflow and fewer blockage episodes, which may help support better sleep continuity. Candidacy requires an ENT evaluation.
— Italic summary: Small, consistent steps add up—then escalate care if needed. —
Lifestyle Tips to Restore Energy While You Treat the Sinus Problem
Sleep-position and nighttime strategies
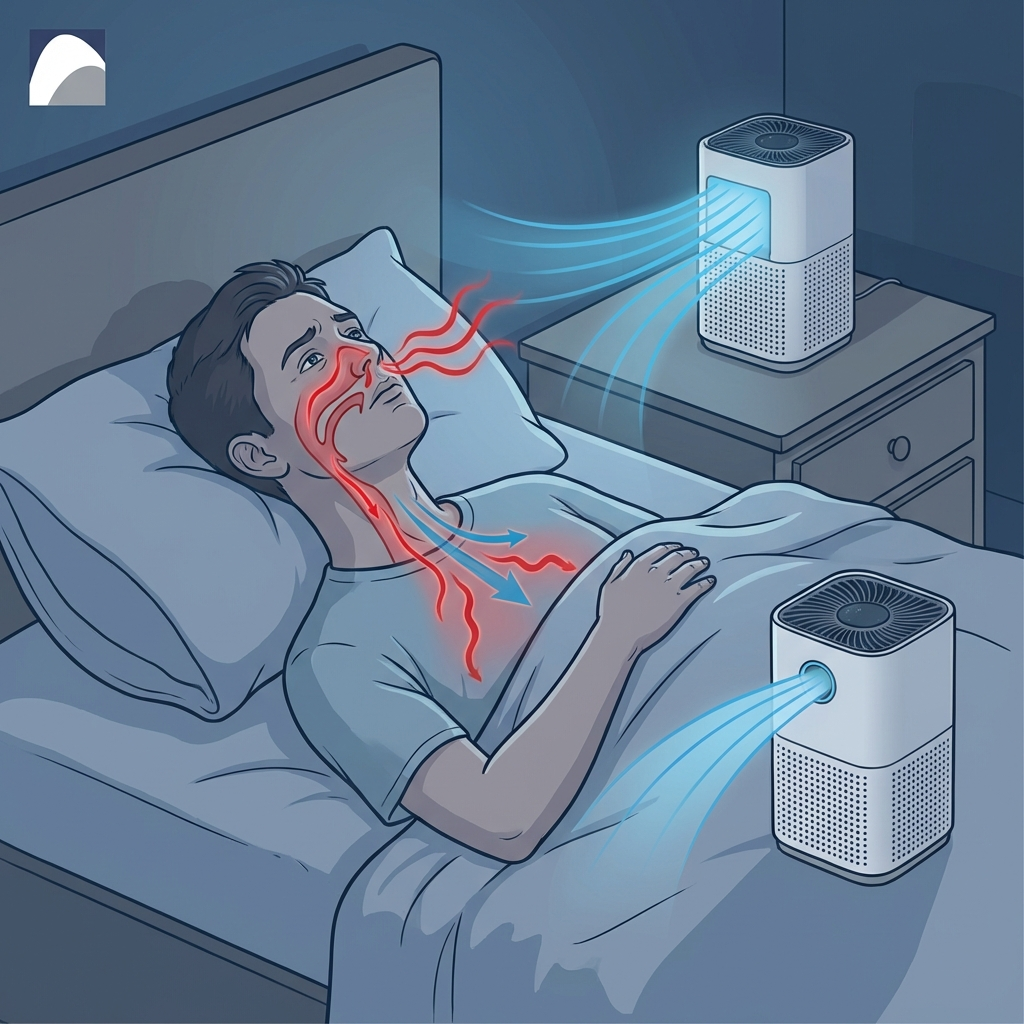
- Slight head elevation may help reduce post-nasal drip and pressure when lying down
- Consider doing saline rinses earlier in the evening so mucus clearance happens before bedtime
- Keep bedroom air cleaner: HEPA filtration, frequent bedding washes, and reducing dust buildup
If you’re waking up with a dry mouth, that can be a sign of nighttime mouth-breathing during congestion. Improving nasal comfort before bed is often more impactful than trying to “push through” with extra caffeine the next morning. For more on sleep impact, visit: https://sleepandsinuscenters.com/blog/how-sinus-issues-affect-sleep-quality-and-ent-solutions
Gentle movement (even when tired)
When fatigue is high, intense workouts can feel impossible. But short walks and light activity can support sleep drive and overall resilience without overtaxing you.
A realistic goal: 10–15 minutes of easy movement most days during a flare. The point isn’t performance—it’s helping your body keep a steady rhythm while you work on the underlying sinus issue.
Hydration + nutrition basics that support mucus clearance
- Adequate fluids can help keep mucus less thick and easier to clear
- Balanced meals support overall health—especially important when fatigue is already present
If your appetite is low, aim for “easy wins” (soups, smoothies, simple proteins) rather than skipping meals, since under-fueling can make fatigue feel worse even when sinus symptoms are improving.
— Italic summary: Support your sleep and recovery while you address the root cause. —
When to See a Doctor (and When to See an ENT)
Seek evaluation if you have:
- Symptoms lasting 12 weeks or more (the chronic sinusitis threshold) (Mayo Clinic)
- Fatigue affecting work, safety, or daily function (including drowsy driving)
- Recurrent “sinus infections” or symptoms that keep returning
Urgent red flags (don’t wait)
Seek urgent evaluation for signs that could indicate complications, such as:
- High fever, severe facial swelling
- Vision changes
- Severe headache, confusion
(General safety guidance consistent with major medical resources such as Mayo Clinic and Cleveland Clinic.)
— Italic summary: Timely evaluation helps target the real drivers of fatigue. —
FAQs
Can chronic sinusitis cause extreme fatigue?
Yes. Fatigue is commonly reported in chronic rhinosinusitis and can significantly impact quality of life (The American Journal of Medicine).
Why do I feel tired even when I sleep 8 hours with sinus congestion?
Total hours don’t always reflect sleep quality. Nasal obstruction and post-nasal drip can fragment sleep and reduce restorative deep sleep, which can leave you exhausted despite “enough” time in bed.
How long does it take to get energy back after treating chronic sinusitis?
Many people notice incremental improvement as congestion reduces and sleep becomes more consistent, but timelines vary depending on triggers (like allergies), anatomy, and which treatments are needed.
Is fatigue a sign of a sinus infection or just allergies?
It can be either. Fatigue is an associated symptom that can occur with chronic sinusitis and with allergies, often through congestion, inflammation, and sleep disruption.
Does balloon sinuplasty help with fatigue?
It may help indirectly for appropriate candidates by improving sinus drainage and nasal airflow, which can support better sleep and reduce the day-to-day burden of symptoms. Outcomes vary; an ENT evaluation is the best way to determine fit.
Conclusion — Treat the Cause, Not Just the Tiredness
If you’re stuck in a loop of congestion, poor sleep, and low energy, the connection between chronic sinusitis and fatigue is real—and addressing sinus inflammation and airflow can make a meaningful difference. A stepwise approach often works best: home routines (like nasal irrigation) and trigger control, then targeted medications and allergy management, and finally ENT evaluation for persistent symptoms or blockage.
To explore personalized next steps, book an appointment with Sleep and Sinus Centers of Georgia: https://www.sleepandsinuscenters.com/
— Italic summary: Your energy often improves when your sinuses do. —
References
- Mayo Clinic — Chronic sinusitis overview: https://www.mayoclinic.org/diseases-conditions/chronic-sinusitis/symptoms-causes/syc-20351661
- Cleveland Clinic — Chronic sinusitis: https://my.clevelandclinic.org/health/diseases/17700-chronic-sinusitis
- The American Journal of Medicine — Chronic rhinosinusitis symptom burden (includes fatigue): https://www.amjmed.com/article/S0002-9343(08)00608-6/fulltext
- Vanderbilt University Medical Center (VUMC) — Fatigue as an indicator in sinus infection context: https://news.vumc.org/reporter-archive/fatigue-strong-indicator-of-sinus-infection/
Medical disclaimer
This article is for general education and is not a substitute for medical advice, diagnosis, or treatment. If you have persistent or severe symptoms, or any urgent red flags, seek prompt care from a qualified clinician.
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.







