How the Immune System Affects Sinus Health: Key Connections and Tips
Introduction: Why your immune system matters for your sinuses
Your sinuses are air-filled spaces around your nose and eyes. They’re lined with a thin, moist membrane that makes mucus and helps trap germs and irritants before they get deeper into your airway.
A common misconception is that sinus trouble is always “just an infection.” In reality, immune function can influence how often symptoms show up, how intense they feel, and whether inflammation becomes chronic. Think of your immune system as the “decision-maker” at the front door: it helps determine whether an exposure turns into a quick cold, a lingering sinus flare, or weeks of swelling and congestion.
That’s why the connection between the immune system and sinus health matters—whether you’re dealing with seasonal flare-ups or symptoms that keep returning.
In this guide, you’ll learn what healthy sinus function looks like, how immune underactivity or overactivity can drive symptoms, what to watch for, and how sinus issues are commonly evaluated and treated (plus practical lifestyle tips and FAQs).
Your immune system helps decide whether a sinus exposure fades fast or turns into a lingering problem.
Quick sinus refresher—what “healthy sinus function” looks like
The sinus lining’s job: filter, humidify, and trap germs
A healthy sinus lining is designed to:
- Humidify and warm the air you breathe
- Trap particles like dust, pollen, smoke, and microbes in mucus
- Move mucus out using tiny hairlike structures called cilia
When cilia and mucus are working well, your sinuses clear themselves quietly—most of the time you don’t notice them at all.
A helpful analogy: your sinuses are like a self-cleaning conveyor belt. Mucus catches what you inhale, and cilia steadily move that mucus “outbound” toward the throat so it can be swallowed without drama.

The immune system’s role on the front lines
Your nose and sinuses are a “front door” for the immune system. Local immune defenses help decide whether an exposure becomes:
- “No big deal,”
- a short-lived viral illness, or
- a longer-term inflammatory problem.
Research on chronic rhinosinusitis shows how immune signaling in the nasal lining can shape ongoing inflammation and symptom patterns.
Healthy sinuses act like a self-cleaning filter—when cilia and mucus flow, symptoms stay quiet.
Key connection #1 — Weakened immunity can mean more sinus infections
What happens when the immune response is underpowered
When the immune response is weaker than it should be, the body may have a harder time clearing viruses or bacteria efficiently. That can allow symptoms to linger or make you more prone to recurrent sinus infections after common colds.
A clinician might describe it like this: “When your immune system can’t finish the job, a routine cold can keep the nasal lining inflamed long enough to block drainage—then everything backs up.”
Signs you might be dealing with recurrent or persistent infections
Patterns that may raise clinician suspicion that your immune function is influencing sinus symptoms (a descriptive concept, not a formal diagnosis) include:
- Multiple sinus infections per year
- Symptoms that last longer than expected
- Infections that improve but then return quickly
- More intense symptoms after routine colds
Concrete example: if you catch a cold, start to feel better, and then congestion/pressure ramps back up for another stretch—especially repeatedly over a year—your clinician may want to look beyond “bad luck.”
Who may be at higher risk
Lower immune resilience can happen for many reasons, including chronic medical conditions or certain medications. That said, immune weakness isn’t the only driver—nasal anatomy, allergies, and ongoing inflammation can create similar “repeat infection” patterns.
When immune defenses lag, colds linger and sinus infections can recur.

Key connection #2 — Overactive or misdirected immunity can drive chronic sinus inflammation
Chronic sinusitis isn’t always “bacteria that need antibiotics”
Many people assume chronic symptoms automatically mean bacteria are stuck in the sinuses. Often, chronic sinus inflammation is driven by immune overactivity rather than persistent bacterial infection. Bacteria can still complicate chronic cases at times, but repeated antibiotics are not always the answer.
A practical way to picture this: antibiotics target bacteria, but they don’t “unclog the drain.” If swelling is the main issue, the priority is reducing inflammation so mucus can move again.
Common immune “triggers”
Immune overreaction can be set off by:
- Allergens (pollen, dust mites, mold, pet dander) — often showing up as allergy-related sinus inflammation
- Irritants (smoke, strong fragrances, air pollution)
- Normal microbes in the nasal environment that, in some individuals, trigger an outsized immune response
Real-life examples patients often notice: symptoms that spike after cleaning with strong sprays, spending time in a dusty basement, or during high-pollen weeks—even if no one else at home is sick.
What chronic inflammation does inside the nose
Inflammation causes swelling in the nasal lining. When that swelling narrows drainage pathways, mucus can get trapped—leading to:
- facial pressure,
- congestion,
- postnasal drip, and
- periodic flare-ups.
Some people describe it as a “pressure cap” over the cheeks or between the eyes, paired with a constant need to clear the throat—classic signs that mucus isn’t draining smoothly.
If you notice symptoms that reliably spike with seasons or exposures, this related article may help: Seasonal sinusitis and immune system: key connections explained (https://sleepandsinuscenters.com/blog/seasonal-sinusitis-and-immune-system-key-connections-explained).
If swelling—not bacteria—is the bottleneck, anti-inflammatory care and drainage support matter most.

Key connection #3 — Autoimmune conditions and genetics: when the immune system targets your own tissues
Autoimmune-linked inflammation in the sinus lining
In some cases, immune dysregulation is broader than allergies alone. Autoimmune conditions can contribute to inflammatory symptoms in multiple body systems—including the upper airway. Medical literature describes links between chronic rhinosinusitis and immune pathways that overlap with autoimmune patterns. Autoimmune involvement is uncommon but may be considered when typical treatments fail or systemic autoimmune symptoms are present.
Genetic links and “inflammation-prone” patterns
Research suggests some people may be genetically more likely to develop persistent inflammatory responses in the nasal lining.
In other words, two people can have the same exposure (pollen, a cold virus, household irritants), but one person’s immune system “stands down” quickly while the other person’s immune system stays activated—keeping tissues swollen and sensitive.
When to raise this possibility with your clinician
It may be worth discussing a broader immune/inflammatory picture if you have chronic sinus symptoms plus systemic symptoms that may suggest autoimmune or systemic inflammatory issues, such as:
- ongoing fatigue,
- joint pain,
- rashes, or
- unexplained fevers,
especially when sinusitis doesn’t respond as expected.
Autoimmune involvement is uncommon but worth considering when symptoms are atypical or systemic.
Key connection #4 — Immune deficiencies (sometimes overlooked in chronic/recurrent sinusitis)
What “immunodeficiency” can look like in real life
Some people experience a pattern of infections that suggests the immune system may not be mounting an effective defense. In day-to-day life, that may look like:
- repeated sinus infections,
- frequent bronchitis, or
- infections that require multiple rounds of antibiotics.
Infections that occur more often or more severely due to weakened immunity are sometimes referred to as sinus infections related to immunodeficiency.
When testing might be recommended
Clinicians may consider immune evaluation when there’s a consistent pattern such as frequent infections, severe infections, unusual organisms, or poor response to standard treatment.
A common “gut check” patients mention is: “I’m doing everything right, but I’m always sick.” That doesn’t confirm immune deficiency, but it’s often a reason to ask whether additional evaluation makes sense.
What evaluation may include (high-level)
An evaluation often starts with:
- reviewing your infection history and timing,
- looking for patterns and triggers,
- and ordering basic labs (for example, immunoglobulin levels and vaccine-response testing), when appropriate.
Frequent, hard-to-clear infections may warrant an immune evaluation.
Symptoms: immune-related sinus problems to watch for
Common sinus symptoms (infections or inflammation)
Many sinus problems—whether infection-driven or inflammation-driven—share the same core symptoms:
- nasal congestion/stuffy nose
- thick drainage or postnasal drip
- facial pressure/pain
- reduced smell/taste
- cough (often worse at night), sore throat from drip
For a broader overview, see: Symptoms of sinus problems (https://sleepandsinuscenters.com/symptoms-of-sinus-problems).
Clues it may be more “inflammation” than “infection”
Signs that point toward a chronic inflammatory pattern include:
- symptoms lasting more than 12 weeks
- frequent flare-ups tied to allergy seasons or exposures
- minimal fever, but recurring congestion/pressure
Red flags—seek urgent care
Sinus complications are uncommon, but it’s helpful to know urgent warning signs:
- swelling around the eye or vision changes
- severe headache with stiff neck or confusion
- high fever, or symptoms that worsen after initial improvement
Track timing, triggers, and duration—these clues help distinguish infection from chronic inflammation.
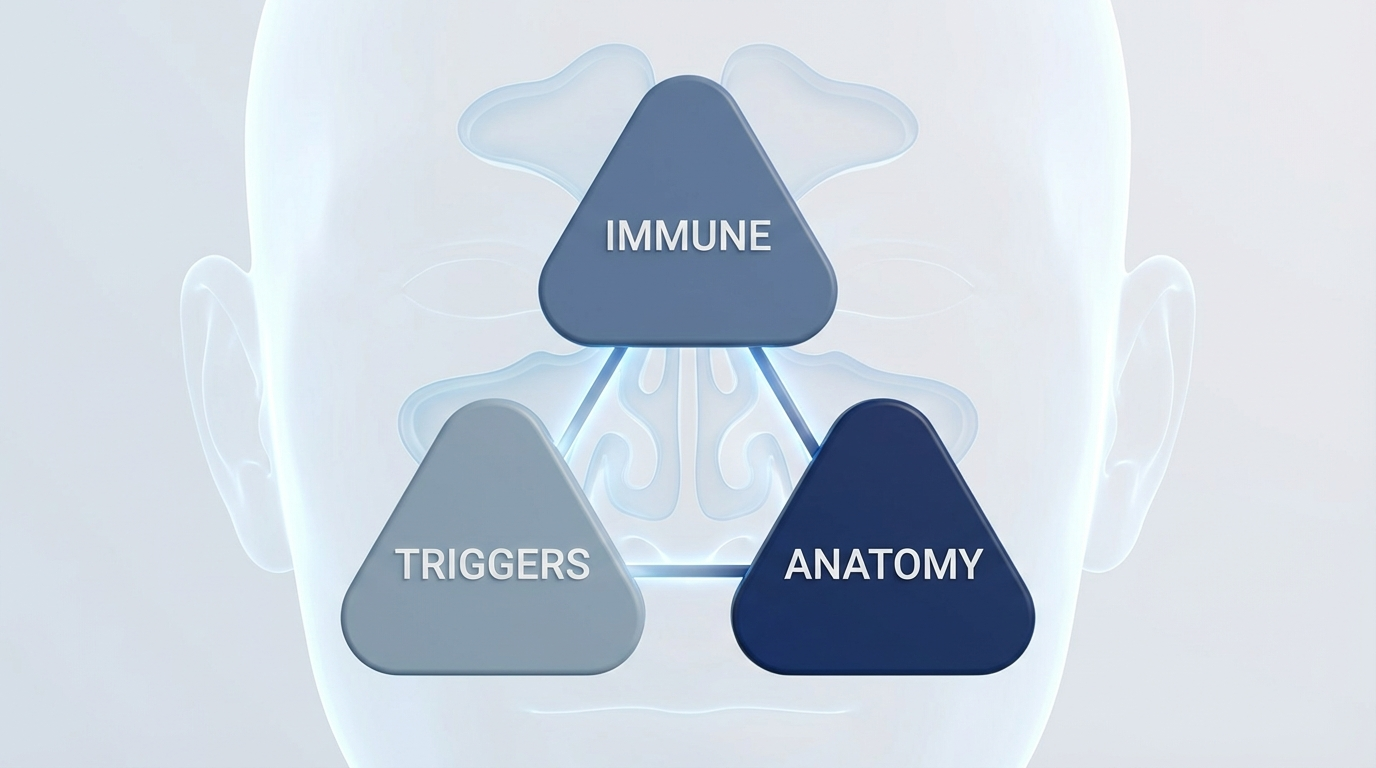
Causes: putting the puzzle together (immune + triggers + anatomy)
The “3-part model” that often explains chronic sinus issues
Many long-running sinus problems come from a combination of:
1) Immune function (underactive vs. overactive/dysregulated)
2) Triggers (allergens, irritants, microbes)
3) Drainage issues (swelling, polyps, deviated septum, narrow passages)
Even when immunity plays a central role, anatomy can keep inflammation going by blocking airflow and drainage. If you suspect a structural contributor, this may be useful: Deviated septum relief (https://sleepandsinuscenters.com/deviated-septum-relief).
Common trigger examples patients can identify
- pollen surges; dusty indoor environments; moldy spaces
- smoke and strong scents
- frequent colds from close-contact settings
This is the practical side of the immune system and sinus health connection: identifying what keeps the immune system “activated” in your nose.
Most chronic sinus issues reflect a mix of immune drivers, triggers, and drainage anatomy.
Treatments: what actually helps when immunity affects sinus health
This section is educational and meant to help you understand common options and why they’re used.
At-home relief (support the lining + improve drainage)
Common supportive strategies include:
- Saline rinses/sprays (using proper technique and safe water)
- Humidification if indoor air is dry
- Hydration and other mucus-thinning habits
For safety details, see: Neti pot safety tips: essential steps for safe nasal irrigation (https://sleepandsinuscenters.com/blog/neti-pot-safety-tips-essential-steps-for-safe-nasal-irrigation).
Medical treatments your clinician may recommend
Depending on whether symptoms look infection-dominant or inflammation-dominant, common options include:
- Nasal steroid sprays to reduce swelling (often used in chronic rhinosinusitis)
- Allergy management, such as antihistamines, nasal antihistamines, and trigger reduction
- Antibiotics are generally reserved for infections suspected to be bacterial and are not routinely used for chronic inflammation-driven sinus symptoms
If you want a clearer breakdown, this guide can help: Viral vs. bacterial sinus infections: key differences (https://sleepandsinuscenters.com/blog/viral-vs-bacterial-sinus-infections-key-differences).
Addressing allergic triggers (immune overreaction)
Because allergies are an immune overreaction to normally harmless substances, targeted allergy care can reduce inflammation and flares. Testing can help clarify what’s driving symptoms: Allergy testing (https://sleepandsinuscenters.com/allergy-testing).
If immune deficiency is suspected
When infection patterns suggest reduced immune defense, clinicians may recommend referral for a focused immune work-up and a prevention plan (for example, reviewing vaccinations and infection-risk reduction strategies).
ENT procedures when blockage/drainage problems keep inflammation going
If symptoms persist despite appropriate medical therapy, an ENT evaluation may look for structural issues or nasal polyps. Treatment options range from in-office procedures to surgery, depending on findings and severity. Learn more here: Chronic sinusitis (https://sleepandsinuscenters.com/chronic-sinusitis) and Acute vs. chronic sinusitis: key differences and treatment options (https://sleepandsinuscenters.com/blog/acute-vs-chronic-sinusitis-key-differences-and-treatment-options).
Match treatment to the driver: reduce inflammation, open drainage, and reserve antibiotics for suspected bacteria.

Lifestyle tips that support immune function and sinus health
Sleep: your immune system’s “overnight reset”
Sleep supports immune regulation and helps the body recover from inflammatory stress. Practical supports include:
- keeping a consistent sleep schedule,
- using a humidifier if the air is dry,
- and building an allergy-aware bedroom routine (clean bedding, reducing dust buildup).
Stress management to support immune balance
Long-term stress may influence immune balance and potentially worsen symptom flare-ups. Options many people find sustainable include:
- walking or light movement,
- brief breathing exercises,
- counseling support,
- a small daily “decompression” habit.
Nutrition basics (immune-supportive, inflammation-aware)
A balanced pattern tends to be most practical: protein + fiber + colorful plants + healthy fats. Some people also notice personal triggers (like dehydration or alcohol) that worsen congestion or postnasal drip.
Exercise: immune-supportive without overdoing it
Regular, moderate activity supports immune function overall. Many people find it helpful to adjust intensity during acute illness and return gradually.
Reduce exposures that keep the immune system “on”
- avoid smoke exposure when possible
- limit strong fragrances/cleaning fumes if they trigger symptoms
- keep indoor humidity in a reasonable range to reduce mold risk
These steps support the immune system and sinus health connection by reducing unnecessary immune activation.
Small daily habits that reduce triggers and support recovery can calm an overactive nasal immune response.
FAQs about immunity and sinus problems
Can a weak immune system cause chronic sinusitis?
It can contribute—especially by making infections more frequent or harder to clear. Chronic symptoms can also come from ongoing inflammation, anatomy, or allergies, so it’s often a multiple-factor situation.
If my sinusitis is chronic, do I automatically need antibiotics?
Not always. Many chronic cases are primarily inflammation-driven rather than an active bacterial infection.
When should I ask about immunodeficiency testing?
It’s reasonable to ask about it if you have frequent or severe infections, need repeated antibiotics, or infections keep returning quickly—especially if there’s a broader pattern beyond the sinuses.
Are allergies an “immune problem”?
Yes. Allergies reflect an immune overreaction to triggers like pollen or dust mites and can inflame nasal and sinus tissue.
What’s the difference between a cold, a sinus infection, and chronic sinusitis?
A cold is usually viral and short-lived. A sinus infection may develop when drainage is impaired. Chronic sinusitis is typically defined by symptoms lasting more than 12 weeks, often with persistent inflammation. For more detail, see: Acute vs. chronic sinusitis: key differences and treatment options (https://sleepandsinuscenters.com/blog/acute-vs-chronic-sinusitis-key-differences-and-treatment-options).
Many sinus issues are multifactorial; personalized care clarifies your main drivers.
When to see an ENT or allergy/immunology specialist
Make an appointment if you have…
- symptoms that repeatedly last >10 days, or continue >12 weeks
- recurrent infections (several per year)
- poor response to standard treatment approaches
- major impact on sleep or quality of life
What to expect at a visit
Visits often include a detailed symptom timeline, trigger review, and (when indicated) an in-office nasal exam/endoscopy or imaging to clarify inflammation vs. infection vs. structural blockage.
If symptoms persist, escalate—evaluation clarifies whether the issue is inflammation, infection, or structure.
Conclusion: A practical takeaway plan
If sinus symptoms keep returning, focus on a clear, stepwise plan:
- Treat today’s symptoms by prioritizing inflammation reduction and drainage support
- Identify triggers, especially allergies and irritants
- Support immune basics (sleep, stress, nutrition, movement)
- Escalate evaluation when patterns suggest chronic inflammation, recurrent sinus infections, or possible immune deficiency
If you’re dealing with persistent or recurrent symptoms, Sleep and Sinus Centers of Georgia can help you sort out the underlying drivers and next steps. To book an appointment, schedule an evaluation here: https://sleepandsinuscenters.com/appointments
A clear plan that fits your pattern beats repeated short-term fixes.
References
- Consultant360. (2013). Chronic sinus inflammation linked to overactive immune system. https://www.consultant360.com/story/chronic-sinus-inflammation-linked-overactive-immune-system
- PMC / National Institutes of Health. (2024). Chronic rhinosinusitis/immune mechanisms. https://pmc.ncbi.nlm.nih.gov/articles/PMC11458559/
- Sinus & Allergy Wellness Center. The role of immunity in chronic sinus problems. https://www.sinusdoctor.com/the-role-of-immunity-in-chronic-sinus-problems/
- My SA Allergist. Chronic sinusitis: Could it be related to immunodeficiency? https://www.mysaallergist.com/post/chronic-sinusitis-could-it-be-related-to-immunodeficiency
- Sleep and Sinus Centers of Georgia. (2025). Seasonal sinusitis and immune system: Key connections explained. https://sleepandsinuscenters.com/blog/seasonal-sinusitis-and-immune-system-key-connections-explained
This article is for educational purposes only and is not medical advice. Please consult a qualified healthcare provider for diagnosis and treatment.
Don’t let allergies slow you down. Schedule a comprehensive ENT and allergy evaluation at Sleep and Sinus Centers of Georgia. We’re here to find your triggers and guide you toward lasting relief.







